Ann Surg:淋巴结转移灶的定位是食管腺癌患者生存的独立预测因子
2016-08-06 Mechront 译 MedSci原创
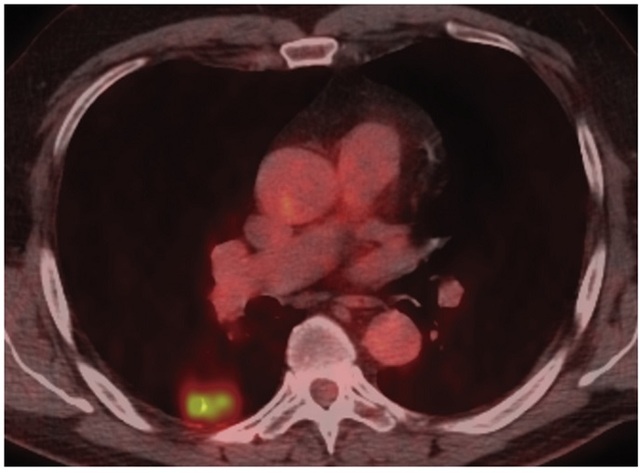
目的:上纵隔及腹腔动脉新辅助治疗和切除后发现淋巴结转移不改变食管癌的TNM分类。这些遥远的淋巴结转移对生存的影响仍不清楚。因此研究者进行了研究,探究食管或胃食管交界(GEJ) 腺癌患者新辅助治疗后食管切除术治疗患者,淋巴结转移位置的预后意义。方法:纳入2003-3至2013-9的479例食道远端或GEJ腺癌患者,进行了新辅助化疗后经胸食管切除术,根据切除标本淋巴结阳性定位,分析生存期。结果:253
目的:上纵隔及腹腔动脉新辅助治疗和切除后发现淋巴结转移不改变食管癌的TNM分类。这些遥远的淋巴结转移对生存的影响仍不清楚。因此研究者进行了研究,探究食管或胃食管交界(GEJ) 腺癌患者新辅助治疗后食管切除术治疗患者,淋巴结转移位置的预后意义。
方法:纳入2003-3至2013-9的479例食道远端或GEJ腺癌患者,进行了新辅助化疗后经胸食管切除术,根据切除标本淋巴结阳性定位,分析生存期。
结果:253例患者有淋巴结转移的切除标本。这些患者中,92例患者局部区域节点淋巴结转移,中位无病生存期为35个月;114例患者树干节点淋巴结转移,中位无病生存期为16个月;21例患者胸部近端淋巴结转移,中位无病生存期为15个月;26例患者树干节点和胸部近端均有淋巴结转移,中位无病生存期为8个月;而没有淋巴结转移的患者,其中位无病生存期为170个月。在多因素分析中,淋巴结转移的位置与生存独立相关。
结论:淋巴结转移灶的定位是生存的独立预测因子。因此,在以后应将淋巴结转移位置纳入食管和GEJ腺癌分期系统中。
原始出处:
Anderegg MC.et al.Prognostic Significance of the Location of Lymph Node Metastases in Patients With Adenocarcinoma of the Distal Esophagus or Gastroesophageal Junction.Ann Surg. 2016 Aug 4. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#食管腺#
75
#转移灶#
88
#患者生存#
77
深度好文,值得学习
141
不错哦,会学到很多
121
很好,不错,以后会多学习
117
深度好文,赞一个!!!
161
继续关注
136
继续关注
69
继续学习
115