Canadian J Cardiol:避免精神药物心血管不良反应的实用方法
2017-12-05 佚名 大话精神
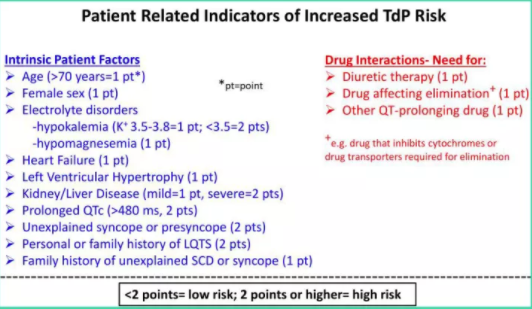
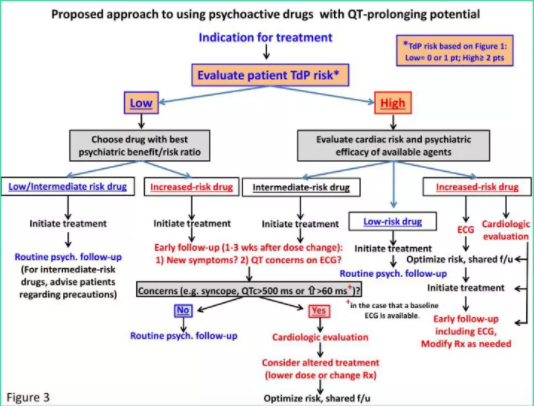
“精神药物”是医学中应用最广泛的药物之一,这些药物可能会影响心血管系统,需要采取适当的预防措施才能安全使用。我们回顾了精神药物对心血管系统的潜在不良后果,并提出一些实用的临床方法以避免这些副作用。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#不良反应#
54
#Cardiol#
46
#DIA#
47
#ANA#
54
学习.了解.了解.
69
不错的.学习了!谢谢分享!
75
学习了.谢谢分享!
90
谢谢学习了.
104
#精神药物#
70
#NAD#
77