Brit J Cancer:PALB2突变与前列腺癌风险和生存率的关系
2021-05-18 MedSci原创 MedSci原创
PALB2突变个体易患侵袭性和致死性前列腺癌。
家族性 PALB2基因的功能缺失性突变是乳腺癌的易感因素,然而,这种突变如何影响男性携带者一生中患前列腺癌的风险尚未明确。近日,肿瘤学领域权威杂志British Journal of Cancer上发表了一篇研究文章,这项研究的目的是明确PALB2突变对前列腺癌风险的作用,并评估PALB2携带者的生存率。

研究人员对5472名未经选择的前列腺癌患者以及8016名男性对照者进行了基因分型,分别确定了两个PALB2突变基因型(c.509_510delGA和c.172_175delTTGT)。在前列腺癌患者中,研究人员将PALB2突变携带者的生存率与非携带者进行了比较。

研究人员在0.29%的前列腺癌病例和0.21%的对照者中发现了PALB2突变(比值比(OR)=1.38;95%置信度区间(CI)为0.70–2.73;p=0.45)。
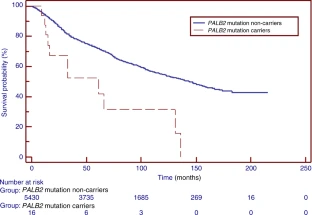
PALB2携带者与非携带者生存曲线
与非携带者相比,PALB2突变携带者更容易被诊断为格里森评分较高(8-10)的侵袭性癌症(64.3 vs. 18.1%,p<0.0001)。晚期高级别前列腺癌的OR为8.05(95%CI为3.57-18.15,p<0.0001)。在中位随访102个月后,与PALB2突变相关的全因死亡经年龄校正的风险比为2.52(95%CI为1.40-4.54;p=0.0023)。PALB2携带者的5年生存率为42%,非携带者为72%(p=0.006)。
由此可见,PALB2突变个体易患侵袭性和致死性前列腺癌。
原始出处:
Dominika Wokołorczyk.et al.PALB2 mutations and prostate cancer risk and survival.Brit J Cancer.2021.https://www.nature.com/articles/s41416-021-01410-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#前列腺癌风险#
87
#癌风险#
80
#生存率#
83
#PALB2#
77
前列腺癌相关研究,学习了,谢谢梅斯
86