病例:导致听力下降的罕见肿瘤
2018-04-16 MedSci MedSci原创
神经瘤多指来自神经鞘组织的神经鞘瘤,主要症状为相关的神经功能障碍及对应神经的渐进性麻痹。但是也有一些症状隐蔽,容易漏诊、误诊的特例。下面要讲的就是一例症状不典型的案例。 左耳闭塞及听力下降 患者为22岁女性,于2个月前无明显诱因下出现左耳不适,有闷塞感,伴听力下降,时有一过性耳鸣,为高调蝉鸣音,休息后略有缓解,无头晕,无耳痛流脓,无面瘫,无吞咽困难、声嘶。自用

神经瘤多指来自神经鞘组织的神经鞘瘤,主要症状为相关的神经功能障碍及对应神经的渐进性麻痹。但是也有一些症状隐蔽,容易漏诊、误诊的特例。下面要讲的就是一例症状不典型的案例。
左耳闭塞及听力下降
患者为22岁女性,于2个月前无明显诱因下出现左耳不适,有闷塞感,伴听力下降,时有一过性耳鸣,为高调蝉鸣音,休息后略有缓解,无头晕,无耳痛流脓,无面瘫,无吞咽困难、声嘶。自用滴耳液滴耳后感耳闷稍减轻,但左耳听力改善不明显。
门诊查体示:,神清,精神良好,心肺(-);神经检查:额纹存在,双侧鼻唇沟对
称,无口角歪斜;耳科检查:双侧耳廓无畸形,右耳鼓膜完整,左外耳道后壁突起一肿物堵塞外耳道,质软,鼓膜不能窥及。
是胆脂瘤还是听神经瘤?
左外耳道听力下降,是听神经瘤?后壁可见肿物突起,是胆脂瘤?根据目前信息基本无法确诊,只能进一步行影像检查:CT平扫显示左侧乳突硬化型,左侧鼓室及乳突窦内可见团块状软组织密度影,密度较均匀,CT值35HU,周围骨质吸收、边缘硬化,窦口扩大,病灶推移听小骨,听小骨结构显示不清,部分骨质吸收破坏,提示:左侧慢性中耳乳突炎,胆脂瘤形成。

增强CT显示左耳乳突软组织占位伴鼓室盖破坏,考虑中耳胆脂瘤;颅内脑实质未见明显异常。

MRI平扫显示左侧乳突炎性肉芽肿。
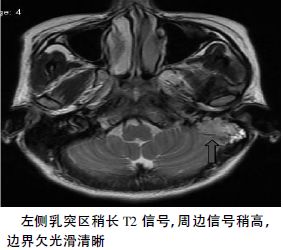
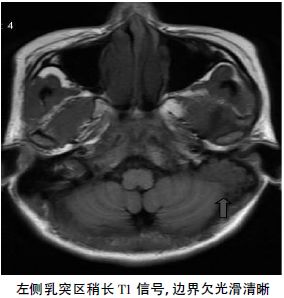
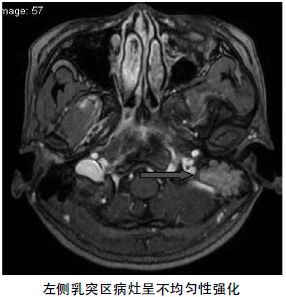
MRI增强显示左侧乳突见一不规则形异常信号灶,大小约29×25×37mm,轮廓不光整,边界较清,T1W呈等信号,T2W呈稍高、低混杂信号影,T2-FLAIR病灶可抑制,DWI信号未见明显增高,增强扫描病灶见不均匀强化,提示:左侧乳突异常信号灶,考虑炎性肉芽肿可能。
病理报告支持哪个?
目前,患者左耳道后壁肿瘤影响患者听力,根据影像结果,符合手术指征,需行手术治疗。故在全麻下行左侧外耳道肿瘤切除术+ 鼓室成形术。
术中见左侧中耳肿瘤呈淡红色,与周围组织界限不清,乳突腔、鼓窦肿瘤向下达乳突尖,后鼓室、下鼓室充满肿瘤,局部骨质吸收破坏,鼓膜受侵犯; 肿瘤从面神经锥段到垂直段沿面神经表面生长,并向下突破且扩大茎乳孔,至二腹肌内; 乙状窦向下至颈静脉球表面骨质被肿瘤破坏吸收。锤骨、砧骨、镫骨尚完整,鼓室黏膜炎性变。术中快速病理结果示“左耳乳突”梭形细胞肿瘤( 神经源性) 。术中清除乳突、鼓室、鼓窦内病变组织,行面神经减压,并用颞肌筋膜覆盖裸露的面神经,颞肌筋膜行内植法修补鼓膜穿孔。
根据术中所见及病理结果,不是胆脂瘤,也不是听神经瘤。患者虽然无面神经症状,但是病理回报为神经源性肿瘤,且沿面神经生长,故可判断为面神经瘤。
手术顺利,术后患者出现面瘫,根据House-Brackman 面神经评级系统,该患者术后面神经功能为Ⅲ级。于术后一周抽除外耳道填塞抗生素纱条,耳后切口愈合良好。
术后病理结果镜下所见 : “瘤细胞梭形丛状结构,部分呈栅栏排列,瘤细胞异形不明显,但见小灶出血坏死”。提示: “左中耳”神经源性梭形细胞瘤。

讨论:
1.面神经瘤比较罕见。一般为良性,临床上一般面神经鞘膜瘤比较多见,面神经纤维瘤和面神经鞘膜瘤各占5%左右。面神经瘤可发生于面神经走形的全程,无特异性的临床症状,故临床诊断相对比较困难。临床表现主要是面神经功能障碍,典型的临床表现是缓慢渐进性面神经麻痹; 第二个常见临床表现是听力下降、耳鸣、耳痛和眩晕等症状。面神经瘤有部分患者症状隐蔽,容易漏诊、误诊。对于怀疑面神经瘤患者,应进行系统的耳神经学检查和颞骨、颅脑CT 扫描以排除面神经瘤。
2.本例患者一般情况良好,诉左耳现仍有闷塞感及轻微耳鸣,无咳嗽,无发热。查体: 神清,精神良好,额纹存在,双侧鼻唇沟对称,无口角歪斜。右耳鼓膜完整,左外耳道后壁突起一肿物堵塞外耳道,质软,鼓膜不能窥及。右耳听力正常。颅脑增强CT检查示“左耳乳突软组织占位伴鼓室盖破坏,考虑中耳胆脂瘤; 颅内脑实质未见明显异常”。根据其病史及相关检查,该患者左耳新生物考虑为中耳乳突占位,不排除胆脂瘤。胆脂瘤是由于鼓膜、外耳道的复层鳞状上皮经穿孔向中耳腔生长堆积成团块,其外层由纤维组织包围,内含脱落坏死上皮、角化物和胆固醇结晶,非真性肿瘤。临床主要表现为间歇性或持续性耳漏和慢性耳钝痛、耳鸣,不同程度的听力下降。检查可见外耳道有白色鳞状上皮样物或干酪样块状物堆积,多有耳道骨壁腐蚀和死骨形成,有些可发现骨缺损。
3.发生于不同部位的面神经瘤需与下列肿瘤鉴别: ( 1) 听神经瘤。临床上较早出现的症状是渐进性听力下降,并可伴有头晕、耳鸣,后期有三叉神经损害、高颅压、小脑功能障碍、脑干受压等症状。因解剖学上的关系,听神经瘤压迫面神经较早,但由于面神经耐受性强,即使被挤压变细,功能仍可较好保留,因此面瘫常出现较晚,且全瘫者少见。( 2) 胆脂瘤。临床上胆脂瘤常有耳漏、耳聋的长期病史,脓有臭味,检查鼓膜常有松弛部穿孔,穿孔处常可看到胆脂瘤皮,不难诊断。但当面神经瘤发生于鼓室段时需与胆脂瘤相鉴别。胆脂瘤是角化扁平上皮组成的囊性团块,常位于上鼓室或鼓窦区。典型的CT表现是上鼓室外壁与听小骨之间有软组织团块,外耳道骨棘、鼓室盾板常有破坏,锤、砧骨向内移位并受侵蚀。( 3) 中耳癌。本病临床表现与面神经瘤不同,中耳癌多合并有慢性化脓性中耳炎,尽管肿瘤侵及面神经管后可引起面神经瘫痪,但早期表现为血性或脓血性耳漏,可有耳深部胀痛,晚期有张口困难、颈淋巴结肿大,极晚期出现Ⅴ、Ⅵ、Ⅸ、Ⅹ、Ⅺ、Ⅻ脑神经瘫痪的各种症状。局部检查时见中耳腔或外耳道有新生物,可取病理鉴别。CT 上可见中耳腔有软组织肿块并有较广泛的骨质破坏,破坏区边缘多呈虫蚀状、不规则,听小骨破坏也较严重。面神经瘤的治疗以手术彻底切除肿瘤为主。保留面神经功能和听力,是防止肿瘤复发,提高生存质量的关键。对于无周围性面神经麻痹的病例,需要通过面神经重建来恢复部分面神经功能。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#罕见肿瘤#
88
#听力#
52
#罕见#
66
阅
86
阅
103