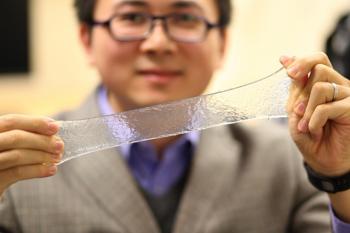
ADV FUNCT MATER:高强高韧矿化水凝胶,颅骨修复的新思路
2017-05-28 佚名 MaterialsViews
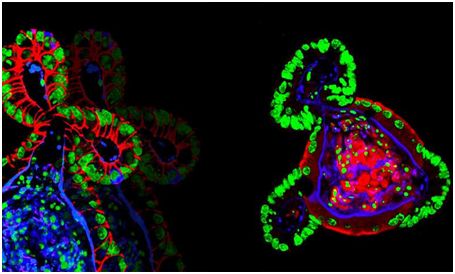
颅骨缺损是最常见和多样性的人类先天性异常之一,严重影响患者的生活质量,特别是创伤、肿瘤切除和血管损伤等造成的大面积的颅骨缺损。目前,颅骨损伤采用的最常见的治疗手段为自体骨和同种异体骨移植。然而,自体骨移植往往面临着形状匹配和来源有限的难题,同种异体骨移植容易引起免疫排斥反应。基于此,很多材料例如生物活性陶瓷、钛网、合成高分子或者它们的复合材料被尝试用于颅骨缺损修复,虽然一定程度上解决了自体和异体骨
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#矿化#
82
#骨修复#
80
#新思路#
97
学习
105
#水凝胶#
65
#凝胶#
80