Blood:提出对地中海贫血中的肺动脉高压患者一种新的筛查手段
2022-06-01 刘少飞 MedSci原创
血液学家必须承担起责任,对地中海贫血患者进行适当的筛查,努力管理他们所控制的风险因素。对地中海贫血有经验的心脏病专家和血液专家需要努力达成共识,而不是临时制定管理指南。
在本期Blood中,WebThal Consortium 的 Pinto 等人介绍了对一组有创记录的肺动脉高压的地中海贫血患者进行了 10 年的重要随访。该研究提出了几个关键发现。首先,即使存在子系统压力,肺动脉高压 (PAH) 也是相当致命的,而且目前的护理标准对患者的治疗不足。其次,超声心动图预测肺动脉压的变化是唯一重要的生存预测指标。
作者的初步报告记录了在地中海贫血中导管插入记录的 PAH 的患病率为 2.1%,比普通人高出10000多倍。然而,通过超声心动图测量的 PAH 患病率至少要高一个数量级。超声心动图出现“假阳性”的原因有很多,但可以通过将三尖瓣反流速度 (TRV) 的阈值调整到更严格的阈值来轻松纠正差异,例如在 3.2 米/秒的阈值中使用WebThal 研究。然而,过于严格的缺点是它将诊断限制在晚期疾病上。在本报告中,诊断后 1、2 和 5 年的 PAH 死亡率分别为 22%、35% 和 40%。WebThal 研究将 3.0 和 3.1 的 TRV 值指定为可能的 PAH,但没有对其进行导管插入或报告其临床结果。鉴于 PAH 的恶性性质,我的临床实践是将右心导管插入术和后续治疗(适当时)扩展到 TRV 速度≥3.0 的患者。TRV 阈值≥3.0 会降低超声心动图的阳性预测值,但会提高潜在可逆性 PAH 的检测。
本报告强调的第二点令人遗憾的是,一旦发现 PAH 在地中海贫血中治疗不足。在本报告中,8 名患者中有 1 名未接受治疗,只有 29.2% 的患者使用了一种以上的药物。尽管 WebThal 研究不足以证明双重治疗的优势,但目前美国胸科医师学会的共识指南建议将 5 型磷酸二酯酶抑制剂和内皮素受体激动剂联合治疗作为有症状患者的一线治疗。3治疗肺动脉高压的三个互补生理轴,一氧化氮、内皮素和前列腺素通路,为药物协同作用创造了充足的机会。内皮素通路也与肾素-血管紧张素-醛固酮轴重叠,产生额外的协同作用。肺动脉高压的序贯附加治疗也是欧洲呼吸学会/欧洲心脏病学会的 1B 类推荐。鉴于多药治疗的复杂性和快速变化的治疗格局,PAH 的地中海贫血患者应转诊至三级中心的肺动脉高压专家,而不是由普通心脏病专家进行管理。
更积极的一点是,最近的 WebThal 研究表明,由 TRV (sPAP = 4 × TRV 2 )预测的收缩期肺动脉压 (sPAP) 趋势代表了跟踪治疗反应的良好生物标志物,与估计相关的 sPAP 改善 25%在研究间隔内存活。这为确定患有 PAH 的地中海贫血患者的治疗升级提供了一个基准。
考虑到WebThal的报告,提出了一个管理算法(见图)。它代表了我的个人观点,但可以作为达成共识准则的起点。建议所有地中海贫血患者进行超声心动图筛查,但筛查间隔要根据患者年龄、基因型、脾脏状况、输血状况和先前的TRV结果来决定。
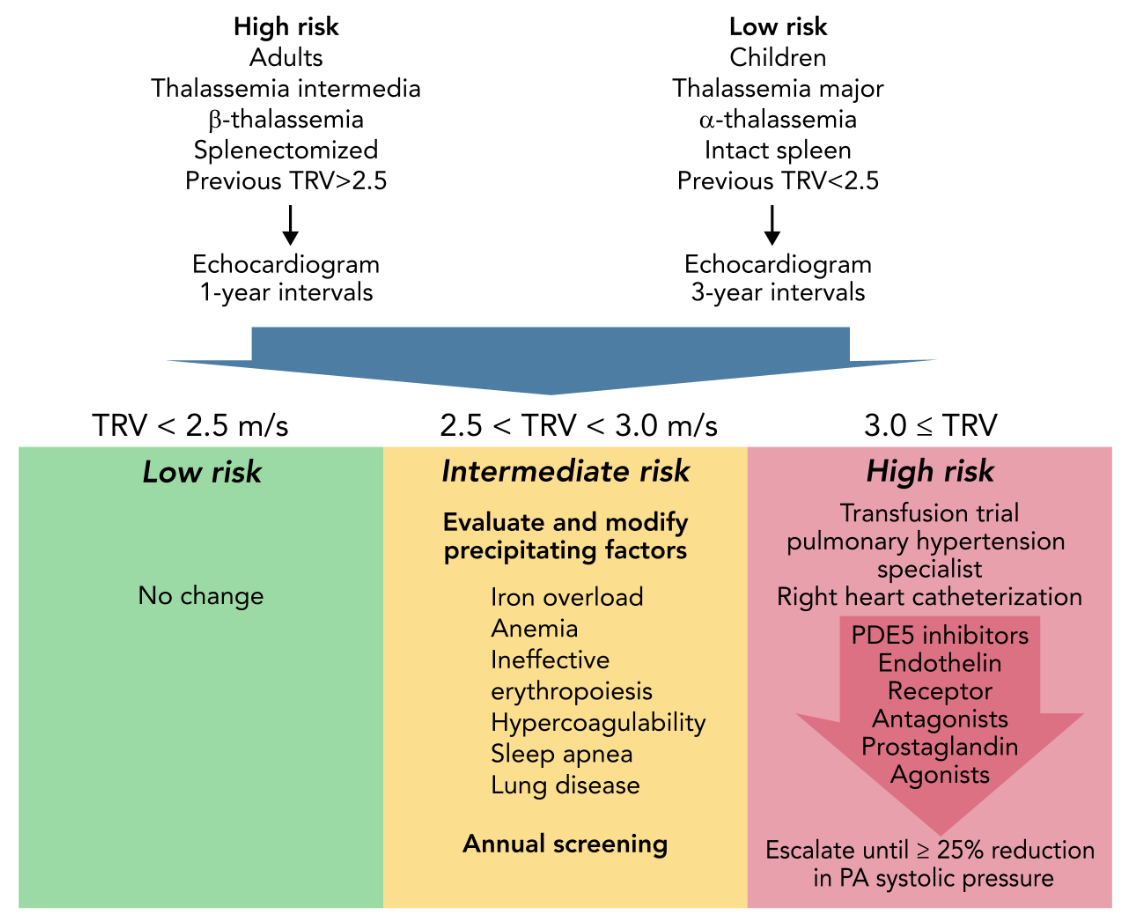
图示,筛查和治疗地中海贫血症肺动脉高血压的拟议算法。代表了由WebThal数据提供的候选肺动脉高血压指南。肺动脉高压的风险随着年龄和脾脏切除而增加,以及贫血和无效红细胞生成的严重程度(受到基因型的影响)。超声心动图检查的频率应反映这些先验风险,以及以前的超声心动图结果。TRV结果<2.5米/秒是正常的,不需要改变监测或治疗。TRV结果在每秒2.5至2.9米之间,表明生理结构异常,有可能发展为肺动脉高压。血液学家必须仔细检查潜在的潜在因素,并尝试改善这些因素,将连续的TRV评估作为成功的生物标志。无论先验肺动脉高压风险如何,记录到的异常TRV超过2.5米/秒就表明是高风险表型,需要每年随访。如果TRV达到每秒3.0米或更高,则表明患者存在导管证实的肺动脉高压的重大风险。第一个关键步骤是开始或加强慢性输血治疗,以完全抑制内源性红细胞生成。在疾病早期,这足以使肺动脉压力恢复正常。如果不成功,应将病人转到肺动脉高压专家处进行右心导管检查,并积极调整肺动脉高压疗法,以达到肺动脉收缩压降低25%的目标。
TRV<2.5米/秒是正常的,不需要改变管理。TR速度为2.5至2.9米/秒,表明生理状态异常,可能是可逆的,在右心导管检查中达到肺动脉高压标准的概率较低。鉴于贫血、无效红细胞生成、铁超载、凝血功能障碍、肺部疾病和睡眠呼吸暂停对肺动脉高压的影响,这个区域的患者需要大量的血液学投入。羟基脲治疗与地中海贫血患者肺动脉压力的超声心动图估计值较低有关。激活素诱导剂或其他改变有效和无效红细胞生成平衡的药物也有可能影响PAH的风险,但在这方面尚未研究。
当TR速度≥3时,绝对有必要进行慢性输血疗法的试验(或完善现有的输血疗法)。在一名地中海贫血患者中,我们通过简单地将输血间隔从6周缩短到3周(未报告数据),成功逆转了导管记录的PAH,其输血标准与重型地中海贫血相同。如果输血治疗失败,应咨询肺动脉高压专家,进行右心导管检查,并开始PAH治疗。在小范围内,西地那非在短期8和长期给药中都显示出疗效。波生坦和静脉注射前列腺素治疗仅在病例报告中有所描述。其他药物,如钙通道阻断剂、曲前列腺素、瓜氨酸环化酶刺激剂和雾化伊洛前列腺素,从未在地中海贫血症中报道过,但在其他形式的肺动脉高压中常规使用。 Pinto等人提出的WebThal数据表明,治疗反应比初始肺动脉压本身更能预测生存率。因此,我建议,治疗方法应该升级,目标是将预测的肺动脉收缩压至少降低25%,必要时使用多种药物来实现这一目标。
这种可怕的并发症的下一步是什么?从基础科学的角度来看,在观察到的临床风险因素和病理生理机制之间仍然存在许多差距。对基本机制的阐明有可能为治疗提供依据。在患者管理方面,由于患者的表型、输血、脾切除的做法以及各地中海贫血中心的监测存在异质性,因此,比较肺动脉高压的发病率和管理的研究具有挑战性。联合研究和病人登记处是研究临床结果的唯一具有成本效益的机制。就个人而言,血液学家必须承担起责任,对地中海贫血患者进行适当的筛查,努力管理他们所控制的风险因素,并将风险最高的患者转介给肺动脉高压专家。最后,对地中海贫血有经验的心脏病专家和血液专家需要努力达成共识,而不是临时制定管理指南。
参考文献:
Wood JC. Pulmonary hypertension in thalassemia: a call to action. Blood. 2022 Mar 31;139(13):1937-1938. doi: 10.1182/blood.2021015340. PMID: 35357479; PMCID: PMC8972095.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








感谢分享
32
#动脉高压#
35
#肺动脉高压患者#
53
#地中海#
49
欢迎关注肺动脉高压研究进展
50
坚持学习
48