JAMA Intern Med:比较新冠肺炎Delta变异株与Beta变异株感染者的临床差异
2021-12-27 MedSci原创 MedSci原创
在卡塔尔Covid-19患者队列研究中,与Beta变异株相比,感染SARS-CoV-2Delta变异后严重不良结局风险增加,未接种疫苗人群患严重危重疾病的几率更大。

随着时间推移,Covid-19疫情迅速演变,新病毒变异株频繁出现。Delta变异株最初在印度发现并在世界范围内迅速传播,目前美国有90%以上的新冠肺炎感染是由Delta变异株引起的。近日研究人员比较了卡塔尔SARS-CoV-2Delta变异病毒感染者与Beta变异感染者的临床结果差异。

研究人员使用卡塔尔国家COVID-19数据库数据,包括所有进行过核酸检测个体数据以及疫苗接种信息,鉴别2021年3月22日至2021年7月7日间确诊的Delta变异株与Beta变异株感染者。研究的主要终点为临床差异,包括入院、进入重症监护病房、补充氧气、使用高流量氧气、接受机械通气以及死亡。
研究期间,总计有1427名患者感染Delta变异株(252名[55.9%]男性;中位年龄34岁)和5353名患者感染β变异株(233名[51.7%]男性;中位年龄34岁),经匹配后确定了451个倾向评分匹配对。与Beta变异株感染者相比,Delta变异株感染者住院(27.3% vs 20.0%)以及中度或重度至危重疾病结局(27.9% vs 20.2%)风险更高。感染Delta变异株与发生任何不良结局风险独立相关(调整后的比值比[aOR]:2.53)。与未接种疫苗相比,在感染前至少3个月完成第二次疫苗接种与Delta变异株感染者(aOR=0.11)和Beta变异株感染者(aOR=0.22)发生任何不良结局的风险降低相关,在感染前完成第二剂疫苗接种不足3个月的患者中,保护作用相似,但仅接种一剂疫苗人群在感染Delta变异体(aOR=1.12)或β变异体(aOR=0.74)后严重不良结局风险增加。
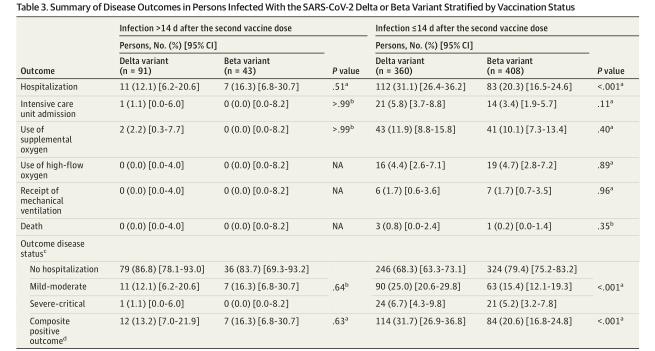
接种疫苗人群感染变异株后的临床结局差异
在卡塔尔Covid-19患者队列研究中,与Beta变异株相比,感染SARS-CoV-2Delta变异后严重不良结局风险增加,未接种疫苗人群患严重危重疾病的几率更大。
原始出处:
Adeel A. Butt et al. Severity of Illness in Persons Infected With the SARS-CoV-2 Delta Variant vs Beta Variant in Qatar. JAMA Intern Med,December 22,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#BET#
58
#变异#
55
#Med#
54