ESC/ERS《肺动脉高压诊断和治疗指南)解读之慢性血栓栓塞性肺动脉高压
2016-08-31 首都医科大学附属北京朝阳医院呼吸与危重症医学科 杨媛华 繆冉 刘岩岩 中华医学杂志
慢性血栓栓塞性肺动脉高压(CTEPH)是以呼吸困难、乏力和活动耐力减低为主要表现的一种疾病,主要由于肺动脉血栓栓塞反复发作、不能溶解,进而导致肺血管重构,肺血管阻力进行性升高、肺动脉高压及右心功能不全。CTEPH的诊断➤ 临床表现CTEPH患者无特异性症状和体征,早期甚至可无症状。常见表现为呼吸困难、咯血、胸痛、晕厥、咳嗽等,仅在晚期阶段右心衰竭的征象才会日益明显。CTEPH 患者的临床
慢性血栓栓塞性肺动脉高压(CTEPH)是以呼吸困难、乏力和活动耐力减低为主要表现的一种疾病,主要由于肺动脉血栓栓塞反复发作、不能溶解,进而导致肺血管重构,肺血管阻力进行性升高、肺动脉高压及右心功能不全。
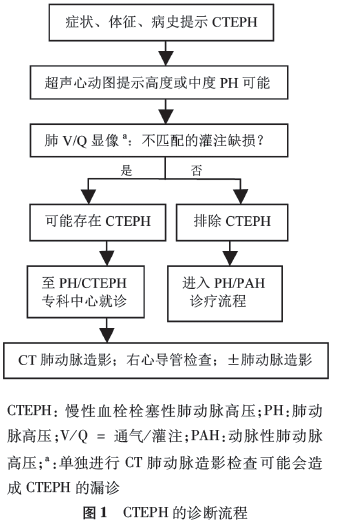
CTEPH的诊断
➤ 临床表现
CTEPH患者无特异性症状和体征,早期甚至可无症状。常见表现为呼吸困难、咯血、胸痛、晕厥、咳嗽等,仅在晚期阶段右心衰竭的征象才会日益明显。CTEPH 患者的临床症状可能与急性肺栓塞或特发性肺动脉高压类似,但水肿和咯血等症状常多见,而晕厥常见于特发性肺动脉高压者。
➤ 辅助检查
(1)指南强调核素肺通气/灌注(V/Q)显 像仍是诊断CTEPH的首选影像学检查方法,敏感度为 96% ~97%,特异度为90% ~95%。
(2) CT肺动脉造影 (CTPA)有助于识别有无疾病的并发症,如肺动脉扩张所致的左冠状动脉主干受压和支气管动脉的扩张,后者可致咯血。需要强调的是仅仅凭借CTPA无法排除CTEPH。
(3)直接肺动脉造影可从前后位和侧位投影充分显示血管的形态,如环状狭窄、血管网(缝)、血管扩张、血管壁不规则、完全性血管闭塞以及支气管侧支循环等情况,并可据此项检査评估手术的可行性。
(4)右心导管术是诊断CTEPH的基本方法。
(5)胸部高分辨率CT (HRCT )可以用来观察肺实质情况,鉴别肺气肿、支气管疾 病或间质性肺病,同时也可以区分肺梗死以及血管、心包、胸 壁畸形等情况。
(6)指南同时指出可根据当地 实际情况和经验进行磁共振成像、电子束CT、血管镜、血管内 超声或光学相干断层扫描等检査,作为诊断的补充。
➤ 诊断标准
CTEPH的诊断需满足以下3条:(1)至少已行3个月的有效抗凝治疗以除外亚急性肺栓塞;(2)右心导管测量平均肺动脉压≥25 mmHg( 1 mmHg =0.133 kPa),同时肺小动脉楔压≤15 mmHg;(3)肺通气灌注扫描显示至 少一个肺段灌注缺损,或多螺旋CTPA、磁共振成像或直接肺 血管造影等检査发现CTEPH的特异性征象,如环状狭窄、网格征/缝隙征和动脉闭塞。
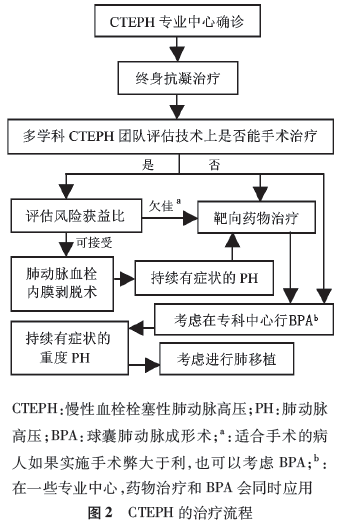
治疗
➤ 手术治疗
肺动脉血栓内膜剥脱术(PEA)仍是 CTEPH首选的治疗方法。
➤ 内科治疗
指南在CTEPH的内科治疗方面更新不多,基本的治疗包括:抗凝、利尿以及对于发生心力衰竭和低氧血症患者进行氧疗。
➤ 介入治疗
介人治疗是2015年指南中首次提及的治疗手段。某些研究显示球囊肺动脉成形术(BPA)治疗可以 改善右心功能,降低肺血管阻力,但导致再灌注肺水肿风险较高,因此BPA应用不是很广泛,应用小球囊结合血管内影像技术进行选择性肺段血管扩张可降低肺水肿风险,目前 BPA术仅应用于有经验的CTEPH中心。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ERS#
78
#治疗指南#
72
#动脉高压#
82
文章很好值得关注
114
继续学习
116
继续关注
115
很好,不错,以后会多学习
128
了解一下
123
继续学习
67
继续关注
61