Eur Urol Oncol:晚期肾细胞癌患者接受一线Pembrolizumab加Axitinib治疗时出现的肝脏毒性的特征和管理
2021-07-27 AlexYang MedSci原创
在KEYNOTE-426(NCT02853331)研究中,Pembrolizumab加axitinib对从未治疗的晚期肾细胞癌的疗效要比比sunitinib更好。然而,3/4级转氨酶升高的发生率却相对
在KEYNOTE-426(NCT02853331)研究中,Pembrolizumab加axitinib对从未治疗的晚期肾细胞癌的疗效要比比sunitinib更好。然而,3/4级转氨酶升高的发生率却相对较高。

近期,有研究人员进一步阐述了接受pembrolizumab-axitinib治疗患者的转氨酶升高的特点。

研究包括了参加KEYNOTE-426的患者。对潜在肝脏疾病的3个标准化MedDRA查询用来鉴定肝脏事件分析亚群(HEAS)的患者。表征了丙氨酸氨基转移酶事件的特点,包括发病时间、恢复时间、皮质类固醇的使用以及对研究治疗的再挑战。
HEAS包括189/429(44%)名Pembrolizumab-axitinib治疗患者和128/425(30%)名Sunitinib治疗患者。3/4级肝脏不良事件在联合治疗组更常见,分别为22%(94/429)与7%(29/425);3%(13/429)的患者因肝脏不良事件而中止联合治疗。在pembrolizumab-axitinib组,125/426名患者(29%)的丙氨酸氨基转移酶(ALT)≥3×正常上限(ULN),发病的中位时间为84天(范围,7-840天)。在ALT≥3×ULN的患者中,120/125(96%)的患者在研究治疗中断/中止后恢复到<3×ULN,恢复的中位时间为15 天(3-176天):68/120(57%)的患者接受了皮质类固醇治疗。100名患者重新接受一种或两种研究治疗,其中45/100(45%)的患者ALT≥3×ULN复发,所有45名患者在研究治疗中断/中止后恢复到ALT<3×ULN。没有发生致命的肝脏事件。
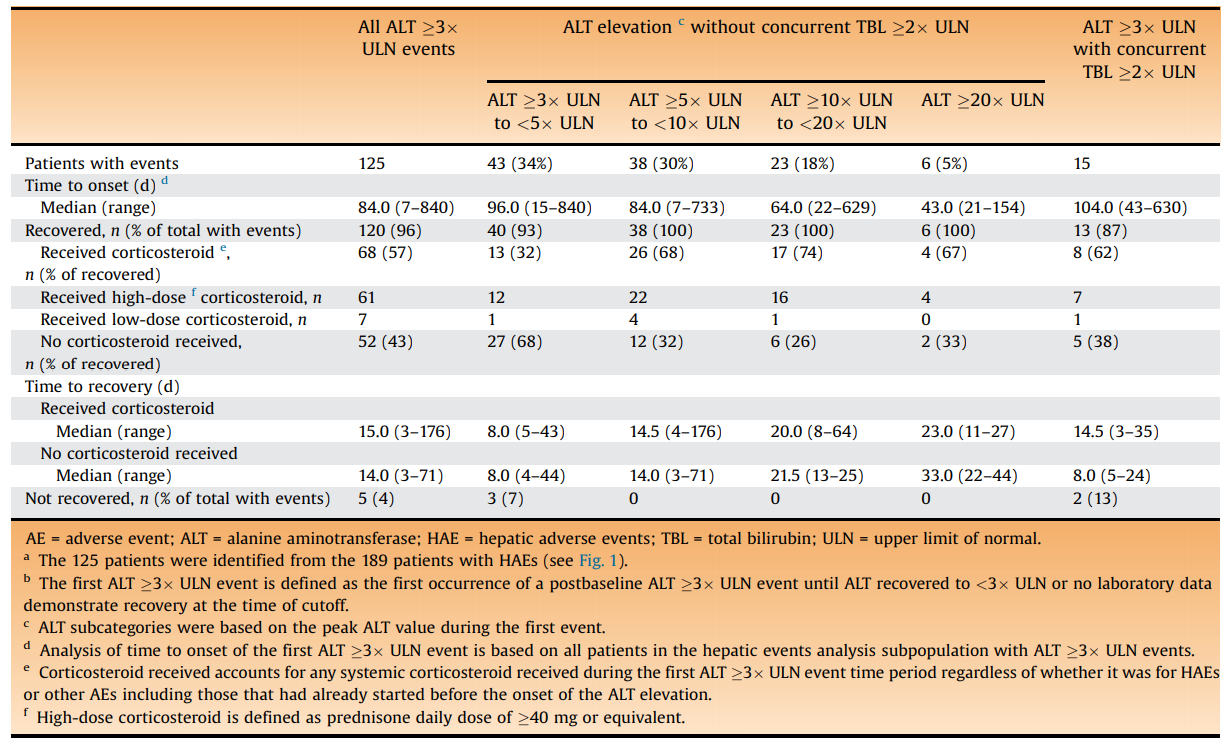
接受pembrolizumab+axitinib治疗患者的首次ALT≥3×ULN事件表征
综上所述,pembrolizumab-axitinib的3/4级转氨酶升高的发生率更高。因此,应仔细评估和处理这些事件,并及时中断或中止研究治疗,并决定是否使用皮质类固醇治疗。另外,重新进行一种或两种药物治疗的决定应基于事件的严重程度和完整的因果关系评估。
原始出处:
Brian I Rini , Michael B Atkins , Elizabeth R Plimack et al. Characterization and Management of Treatment-emergent Hepatic Toxicity in Patients with Advanced Renal Cell Carcinoma Receiving First-line Pembrolizumab plus Axitinib. Results from the KEYNOTE-426 Trial. Eur Urol Oncol. Jul 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#细胞癌#
109
#PE#
70
#mAb#
79
#Pembro#
82
#Oncol#
84
#Pembrolizumab#
75
#晚期肾细胞癌#
69
谢谢梅斯分享这么多精彩信息
88