心血管疾病(CVD)是影响全球人类健康的主要原因,其死亡率占全球年总死亡数的1/3,在高收入国家CVD死亡率为20-50%。心脏康复通过改善心脏病患者的运动耐量和心功能,缓解症状,减少焦虑、抑郁和压力的心理状态,是所有心脏病二级预防的重要组成部分。
无论是稳定性心绞痛、急性冠脉综合征和冠状动脉血运重建术后患者,抑或是慢性心力衰竭、经历过心脏移植或瓣膜置换术的患者均可从心脏康复中获益,可显著降低全因死亡率和心血管死亡率。其中,心脏康复五大处方中的“运动处方”通过改变CVD风险因素分布,改善患者心脏和冠状血管功能,显著降低致死性和非致死性再次心梗的风险。

运动康复能显著改善冠心病和心力衰竭患者的心血管、肺和骨骼肌功能,提高运动耐量,改善生活质量和心理健康(包括抑郁及压力状态)。与连续有氧运动训练相比,高强度间歇训练(HIIT)能更好改善患者的最大有氧能力。
因此近年来,HIIT已被视为低风险患者的一种替代运动方式。最近的荟萃分析显示,在射血分数降低(<40%)的HF(HFrEF)患者中,HIIT比中等强度连续运动(MCE)更能改善摄氧量峰值(VO2peak)。
那么,高强度间歇训练(HIIT)是否比中强度连续训练(MICT)更能改善心肺适应性?究竟指南是不是更适合心衰患者?为此,德国慕尼黑工业大学Martin Halle团队研究了HIIT、MCE或基于指南的体力活动对射血分数保留的HE患者VO2peak的影响。研究结果发表在最新《美国医学会杂志》(JAMA)杂志上。
2014年7月至2018年9月,研究人员在5个城市(德国柏林、莱比锡和慕尼黑;比利时安特卫普;挪威特隆赫姆)进行了随机临床试验。从532名筛选出的患者中,纳入180名慢性、稳定的HFpEF患者。
患者被随机分配(1:1:1;每组n=60)到HIIT(3×38min/w)、MCE(5×40min/w)或指南指导对照组(根据指南提供1次体力活动建议)。该研究共为期12个月(3个月在诊所,然后是9个月远程医疗监督的家庭锻炼)。
该研究的主要终点是3个月后V̇o2峰值的变化。次要终点包括3个月和12个月后患者心肺功能、心脏舒张功能和钠尿肽(BNP)等指标的变化。
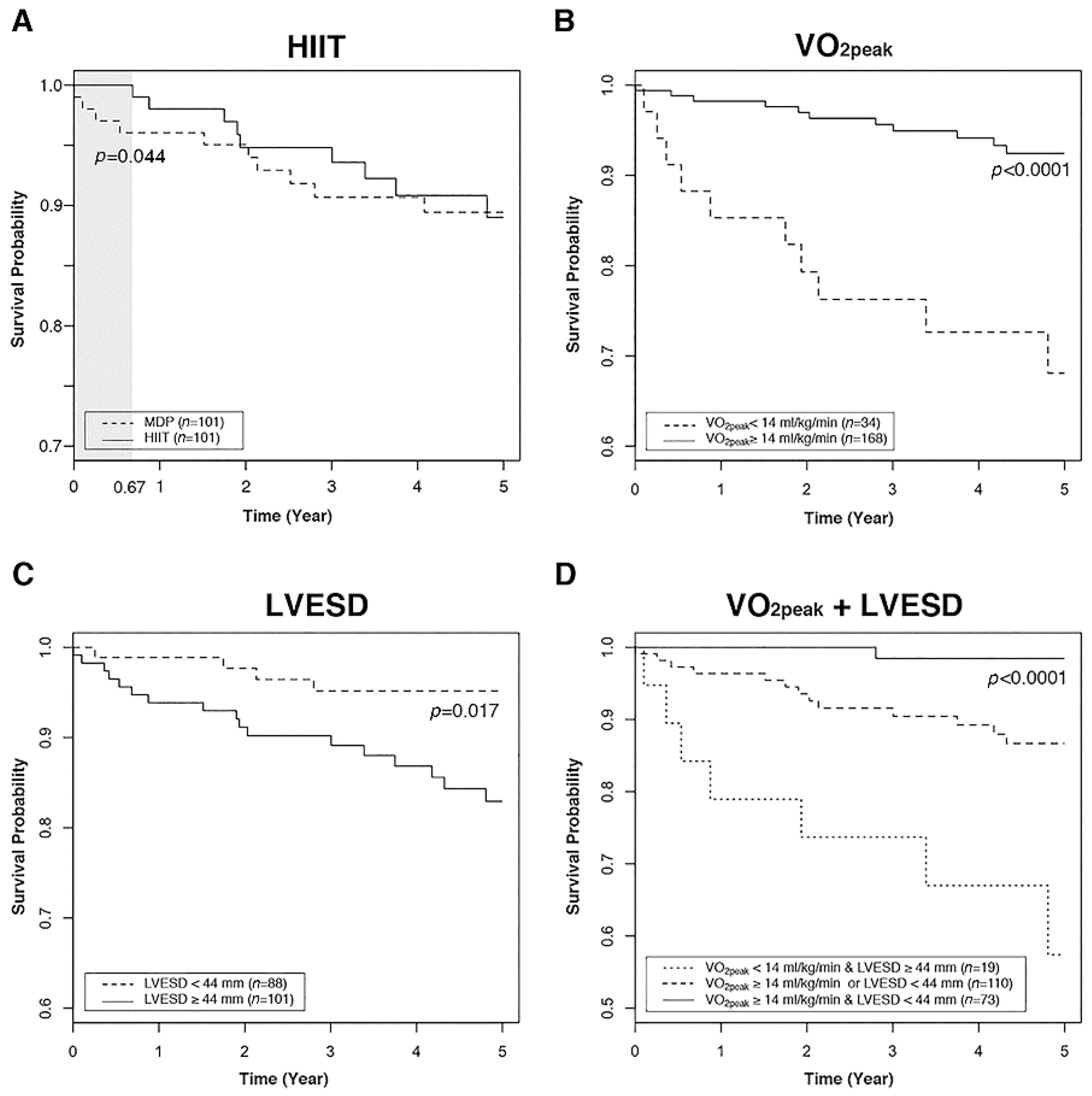
在180名随机化的患者中(平均年龄=70岁;120名女性[67%]),分别有166名(92%)和154名(86%)在3个月和12个月时完成了相关评估。3个月时,HIIT组与指南对照组的峰值V̇o2变化为1.1 vs -0.6 mL/kg/min(差异=1.5[95% CI,0.4~2.7]);MCE组与指南对照组的变化分别为1. 6 vs -0.6 mL/kg/min(差异=2.0 [95% CI,0.9~3.1]);HIIT训练组与MCE阻的变化则为1.1 vs 1.6 mL/kg/min(差异=-0.4 [95% CI,-1.4~0.6])。
然而,在12个月时峰值V̇o2变化则无统计学意义。此外,心脏舒张功能或BNP水平也无明显变化。在该研究过程中,4名HIIT患者(7%)、3名MCE患者(5%)和5名指南对照患者(8%)出现急性冠脉综合征。
在HFpEF患者中,HIIT与MCE在3个月时的峰值V̇o2变化差异没有统计学意义。与指南对照组相比,两组都没有达到预先规定的最小临床重要差异。
综上,这些研究结果提示,HFpEF患者选择HIIT、MCE与基于指南的体力活动获益差异不大。
参考文献:
Mueller S, et al. Effect of High-Intensity Interval Training, Moderate Continuous Training, or Guideline-Based Physical Activity Advice on Peak Oxygen Consumption in Patients With Heart Failure With Preserved Ejection Fraction: A Randomized Clinical Trial. JAMA. 2021;325(6):542–551. doi:10.1001/jama.2020.26812
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JAMA#点击进入话题查看更多相关文章 或评论时插入话题加入讨论
175
#心衰患者#
70
#HIIT#
71
学习了
112
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
70