EBCC-11∣邵志敏教授团队:年轻乳腺癌患者总生存率与疾病特异生存率列线图的构建与验证
2018-03-25 龚悦 肿瘤瞭望
第11届欧洲乳腺癌大会于当地时间3月21日在西班牙巴塞罗那拉开序幕。复旦大学附属肿瘤医院邵志敏团队关于构建年轻乳腺癌患者生存预后风险评估模型的研究入选大会壁报。
年轻乳腺癌是较为特殊的乳腺癌群体,年龄小于40岁的乳腺癌患者约占总体乳腺癌人群的7%左右。既往研究报道年轻乳腺癌相较于年长乳腺癌,恶性程度更高、预后更差。年轻乳腺癌的肿瘤组织学分级相对较高,雌激素受体(estrogen receptor, ER)阴性、孕激素受体(progesterone receptor, PR)阴性以及人表皮生长因子受体2(human epidermal growth factor 2, HER2)阳性的比例也相对较高。
目前在年轻乳腺癌患者治疗策略的选择上仍有许多不明确的地方,包括是否所有的年轻乳腺癌患者都需要接受化疗以及哪些患者可以接受保乳治疗等。因此,根据不同年轻乳腺癌患者的复发与死亡风险进行分组以选择最佳治疗策略是非常重要的。
该研究纳入了1990年至2010年美国监测、流行病学及预后数据库(Surveillance, Epidemiology, and End Results, SEER)中18岁至39岁的非IV期浸润性乳腺癌女性患者共24889名,并随机分为了训练集与验证集,患者的中位生存时间为99个月。
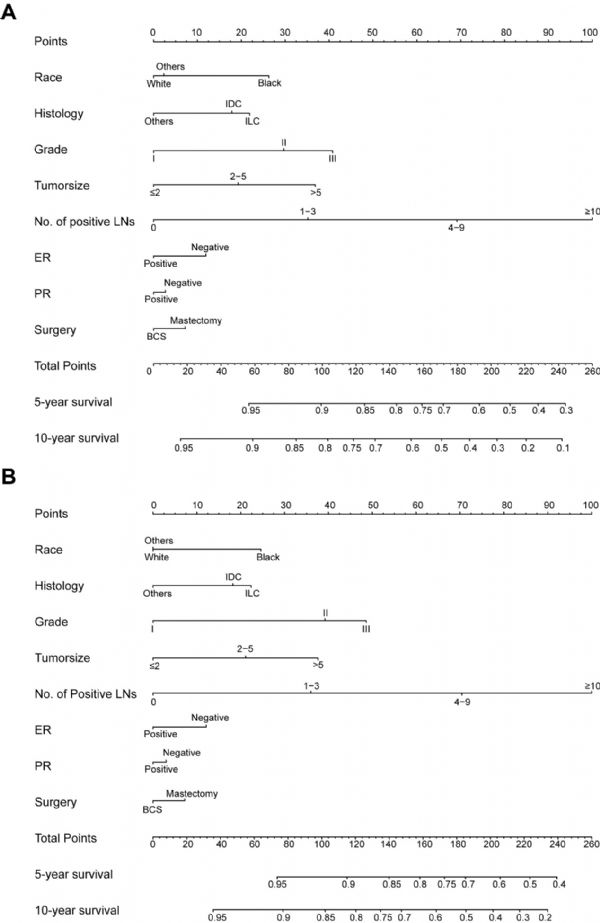
在训练集中,通过Cox回归模型的分析发现种族、组织学类型、组织学分级、肿瘤大小、阳性淋巴结个数、ER状态、PR状态以及手术方式共8项指标是年轻乳腺癌患者的总生存率(overall survival, OS)以及疾病特异生存率(disease-specific survival, DSS)的独立预后因素。基于包含这8项指标的多因素Cox回归模型构建了列线图(nomogram)来预测年轻乳腺癌的5年以及10年的OS和DSS(Figure 1)。
Figure 1
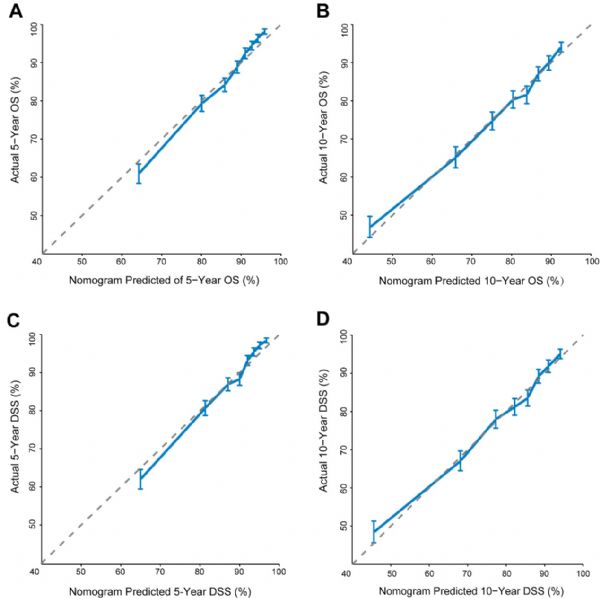
随后该项研究利用校准曲线与一致性指数(concordance index, C-index)对所构建的nomogram进行验证。从训练集的校准曲线上可以看出,nomogram对于5年以及10年OS和DSS的预测结果与实际结果大致相仿(Figure 2),预测OS和DSS的C-index分别为0.720和0.729。同时在验证集中对nomogram的辨别度与校准度的研究也能得到较好的结果。
Figure 2
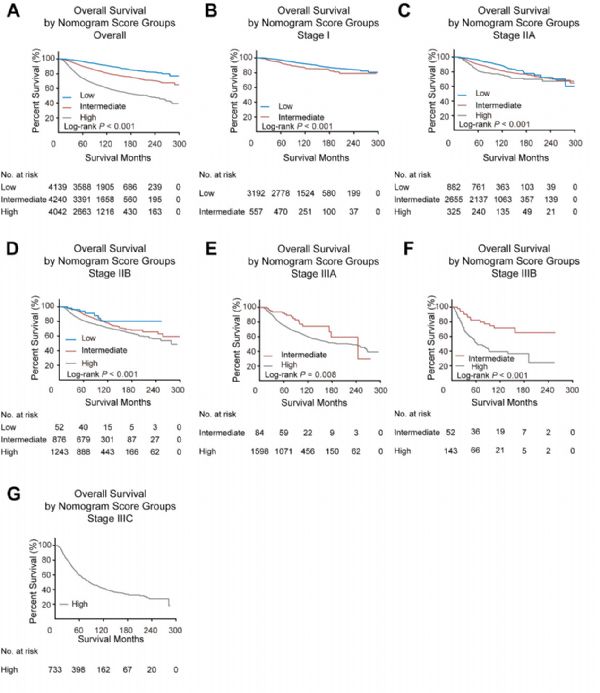
该研究还通过计算每位年轻乳腺癌患者OS的nomogram评分,将患者分成3个不同的死亡风险组,低风险组患者的预后最佳,而高风险组患者的预后最差。不同组之间的预后差异不管是在总人群中还是在不同TNM分期中都有显着的差异(Figure 3)。
Figure 3
本项研究利用一项基于人群的大型数据集,构建并验证了能够用于预测年轻乳腺癌患者OS和DSS的nomogram,并且在训练集和验证集中均验证了nomogram的预测能力。本研究构建的nomogram可以指导临床医生更精确地预测年轻乳腺癌患者个体的预后,并对其中高危风险的人群进行更个体化的治疗。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#列线图#
117
#年轻乳腺癌#
60
很好很好
96
#生存率#
58
#乳腺癌患者#
64