Eur J Cancer:BRCA1/2突变对三阴性乳腺癌新辅助化疗时发生严重血液毒性风险的影响
2021-01-13 xiaozeng MedSci原创
BRCA1和BRCA2在DNA修复中起核心作用。因此,携带胚系(g)BRCA1/2突变(m)的患者接受化疗治疗后,发生血液性毒性的风险可能更高。
BRCA1和BRCA2在DNA修复中起核心作用。因此,携带胚系(g)BRCA1/2突变(m)的患者接受化疗治疗后,发生血液性毒性的风险可能更高。
本研究分析了两个乳腺组研究的早期三阴性乳腺癌(TNBC)患者,这些患者的gBRCA1/2突变状态已知,且均接受蒽环类紫杉醇新辅助化疗治疗。主要目标是第1个疗程(C1)时III-IV级(G)中性粒细胞减少率。次要目标包括C1时对总体和其他GIII-IV级血液学毒性的影响,以及整个周期的累积血液性毒性、相对总剂量强度以及粒细胞集落刺激因子的预防。探讨了紫杉烷、卡铂和环磷酰胺的血液性毒性。
gBRCA1/2突变对发生血液毒性的影响
1171位受检者中有209位(17.8%)携带gBRCA1/2突变。C1时,37.4%的gBRCA1/2突变患者有GIII-IV中性粒细胞减少症,而野生型患者中有35.7%发生了GIII-IV中性粒细胞减少症(P=0.683)。在多变量回归模型中,对于C1,gBRCA1/2m既不能预测GIII-IV中性粒细胞减少症(优势比[OR]1.26,95%CI 0.87-1.82,P=0.226),也不能预测其他GIII-IV血液性毒性(OR 0.91,95%CI 0.64-1.31,P=0.0.625)。对整个周期的累积毒性分析得出了类似的结果,除了GIII-IV血小板减少症(在gBRCAm患者中是增加的)。
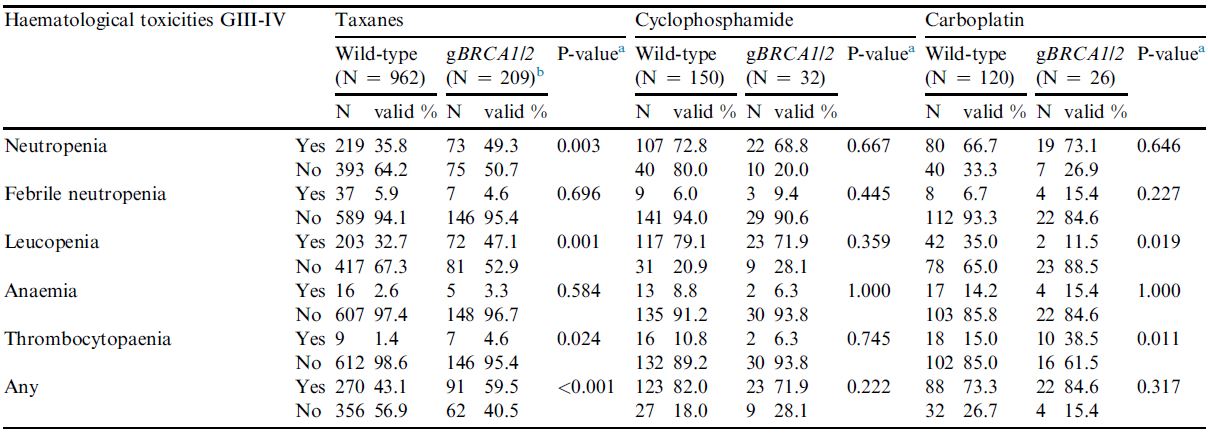
gBRCA1/2突变对不同药物治疗时发生血液毒性的影响
在接受紫杉醇治疗的患者中,gBRCA1/2m患者的GIII-IV血液性毒性的发生率高于野生型(59.5% vs 43.1%;P<0.001)。在采用环磷酰胺或含铂化疗的患者中也未见差异。
在标准化疗下,携带gBRCA1/2突变的TNBC患者在第一个疗程时或在整个治疗周期中累积发生严重血液性毒性的风险并不高。在紫杉醇治疗下,携带gBRCA1/2突变的患者发生GIII-IV血液性毒性的风险可能更高,需要进一步研究。
原始出处:
Furlanetto Jenny,Mobus Volker,Schneeweiss Andreas et al. Germline BRCA1/2 mutations and severe haematological toxicities in patients with breast cancer treated with neoadjuvant chemotherapy. Eur J Cancer, 2021, 145: 44-52.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#阴性乳腺癌#
73
#新辅助#
116
#BRCA1#
97
#三阴性#
70
#BRCA1/2#
123
#BRCA#
104
#BRCA1/2突变#
114