Ann Intern Med:结直肠肿瘤息肉不完全切除后的复发风险
2021-10-06 Nebula MedSci原创
与息肉完全切除的结肠段相比,息肉不完全切除的结肠段的未来瘤变和晚期瘤变风险显著增加
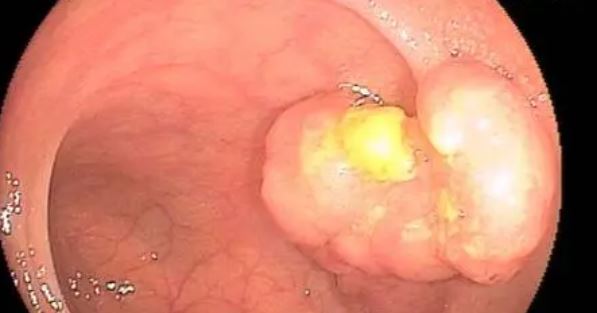
结肠息肉切除不完全被认为是结直肠癌发生的重要原因。据估计,不完全息肉切除占所有结肠镜检查后结直肠癌的10%-30%。但是,目前尚没有关于不完全切除的息肉的自然史数据。
这是一项观察性队列研究,旨在探讨结直肠息肉不完全切除后的复发风险。
受试患者为手术切除5-20 mm肿瘤息肉的有完全或不完全切除记录的结肠息肉患者,予以监测检查。节段性异时性瘤变的定义:首次监测检查时至少有1个肿瘤息肉的结肠节段比例。
受试患者的息肉切除情况
在233位受试患者中,有166位(71%)至少接受过一次监测检查。与息肉完全切除相比,息肉不完全切除后进行监测检查前的中位时间明显缩短(17 vs 45个月)。息肉未完全切除的肠段的异时性肿瘤发生的风险明显高于息肉完全切除的肠段(52% vs 23%;风险差[RD] 28%, 95% CI 9%-47%; p=0.004)。
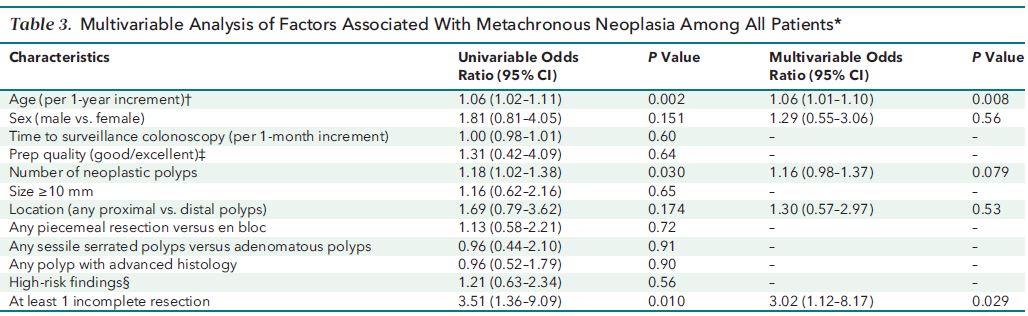
与异时性肿瘤相关的因素
息肉不完全切除肠段复发息肉的数量也更多(平均值 0.8 vs 0.3; RD 0.50, 0.1-0.9; p=0.008),发生晚期腺瘤的风险也更高(18% vs 3%;RD 15%, 1%-29%; p=0.034)。息肉不完全切除是与异时性肿瘤相关的最强的独立因素(优势比 3.0, 95% CI 1.12-8.17)。
综上所述,该研究发现,与息肉完全切除的结肠段相比,息肉不完全切除的结肠段的未来瘤变和晚期瘤变风险显著增加。
原始出处:
Pohl Heiko,Anderson Joseph C,Aguilera-Fish Andres et al. Recurrence of Colorectal Neoplastic Polyps After Incomplete Resection.[J] .Ann Intern Med, 2021, https://doi.org/10.7326/M20-6689
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#复发风险#
68
#直肠肿瘤#
78
#结直肠#
66
#结直肠肿瘤#
95
#Med#
75
风险较高
68
谢谢
83
T裤卡恩来我家玩呢吧台L码头
84
学习了
72