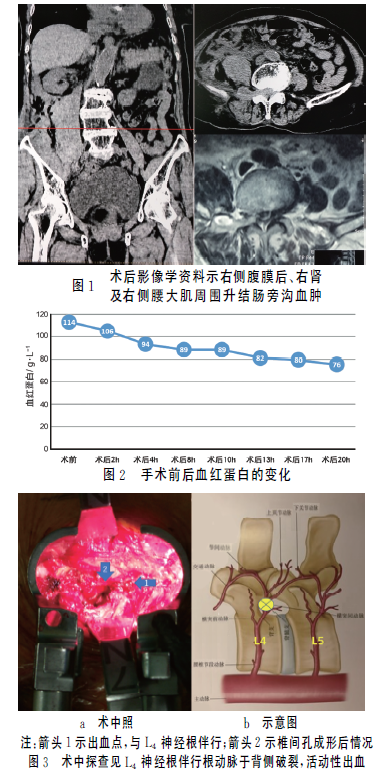
椎间孔镜术后弥漫性腹膜后血肿1例
2018-10-18 张鑫 温勇 杜炎鑫 实用骨科杂志
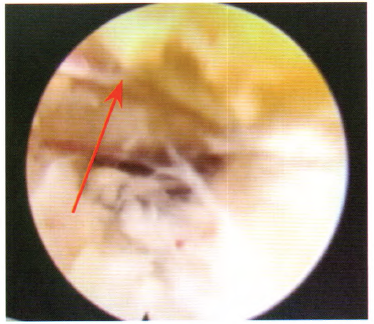
近年来,临床上广泛应用经皮椎间孔镜技术(PELD)治疗腰椎间盘突出症,并取得良好的效果。其创伤小,出血少,恢复快,病人满意度高。血肿形成是PELD术后罕见的并发症,目前国内外关于血肿形成的报道大多行保守治疗,本文报道1例高龄腰椎神经根管狭窄患者行PELD手术,术后发生弥漫性腹膜后血肿并行二次血肿清除术。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#椎间孔镜#
70
#椎间孔#
119
#腹膜后#
68
#血肿#
67
#弥漫性#
53
#腹膜#
75