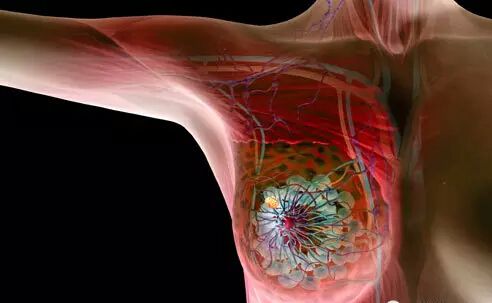
Oncogene:靶向受体蛋白延缓乳腺癌转移
2016-10-07 佚名 生物谷
在一项发表在国际学术期刊Oncogene上的研究中,来自美国迈阿密大学米勒医学院的研究人员通过靶向一种叫做RAGE的受体分子抑制了乳腺肿瘤生长,肿瘤血管生成和炎症细胞的招募,大大减少了乳腺癌细胞向肺和肝的转移。 "RAGE高表达在多种癌症中,与乳腺癌和其他癌症病人的不良预后有关,"文章通讯作者Barry I. Hudson这样说道。"在这项研究中,我们检测了通过多种方法靶

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












继续关注!
44
谢谢分享!
57
好文章,受益
0
文章很好,继续关注
54
#Oncogene#
25
#癌转移#
23
#Gene#
32