JAHA:心脏结节病和特发性巨细胞心肌炎的临床表现和结局比较
2021-03-04 MedSci原创 MedSci原创
GCM与CS的不同之处在于,它具有更广泛的心肌损伤和较差的患者预后。然而,患者预后的关键决定因素似乎是心肌损伤的程度,而不是组织病理学诊断。
心脏结节病(CS)和巨细胞心肌炎(GCM)具有许多相似的组织病理学和临床特征。它们是否是某一种疾病的一部分目前仍无定论。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员比较了自1980年代末以来直至2018年2月期间351例CS病例和28例GCM病例的医疗记录数据,他们发生了心脏死亡、猝死和心脏移植的复合终点。
GCM和CS患者出现心力衰竭表现的比例分别为50% vs. 15%(P<0.001),高级房室传导阻滞分别为21% vs. 43%(P=0.044)。就目前而言,81%的GCM病例中左心室射血分数≤50%,而在CS病例中则为48%(P=0.004)。GCM病例入院时血浆B型利钠肽前体N末端(NT-proBNP)的中位数(四分位数范围)为5273(2782-11309)ng/L,而CS病例为859(290-1950)ng/L(P<0.001),而19例GCM病例中有17例患者心脏肌钙蛋白T超过50 ng/L,而239例CS病例中有48例患者心脏肌钙蛋白T超过50 ng/L(P<0.001)。
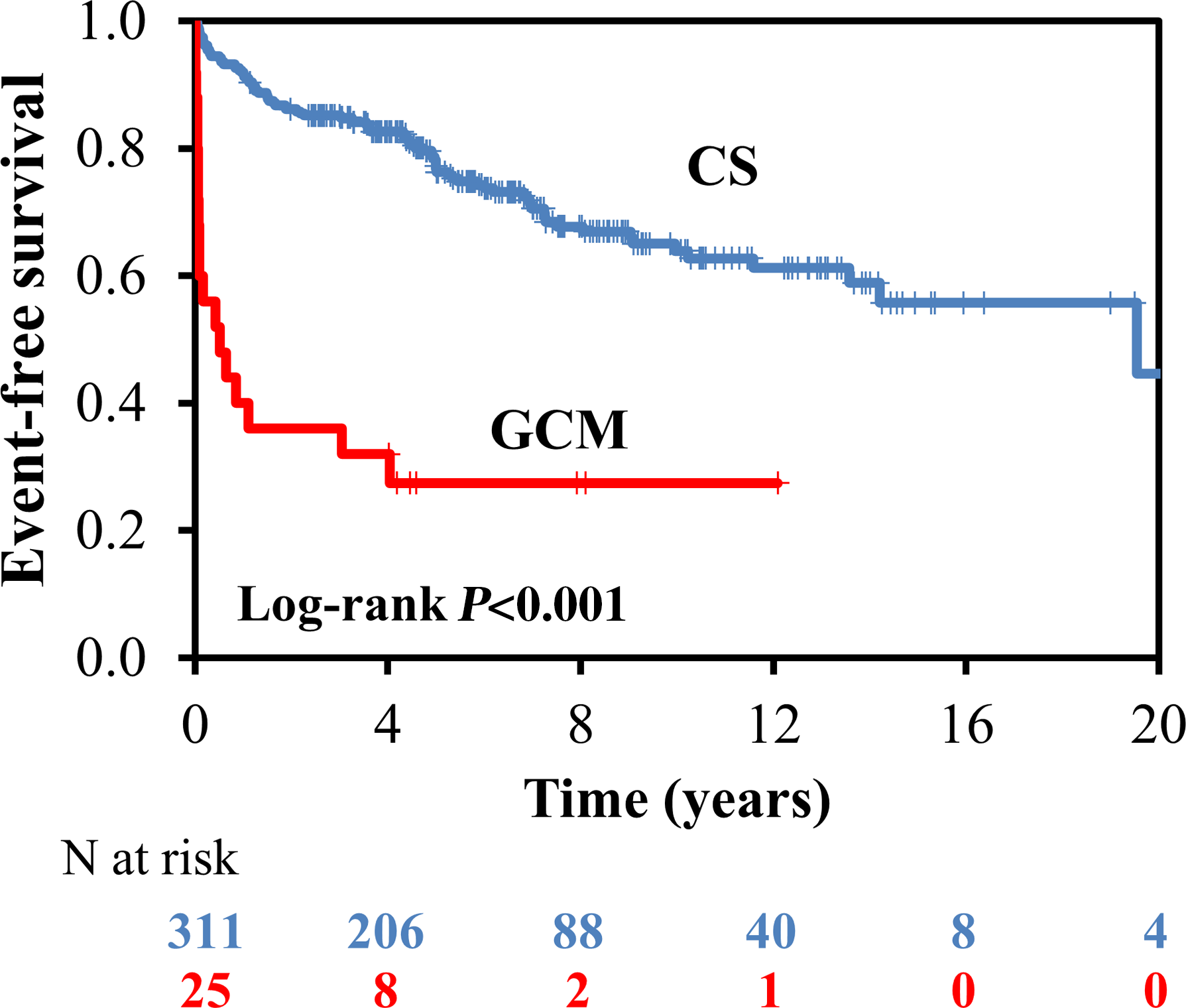
CS病例5年无事件生存率估计为77%(95%CI为72%–82%),而在GCM病例中为27%(95%CI为10%–45%)(P<0.001)。通过Cox回归分析,GCM病例预测的心脏事件危险比为5.16(95%CI为2.82–9.45),但是在纳入心肌损伤和功能障碍标志物后,风险比降低至1.58(95%CI为0.71-3.52)。
由此可见,GCM与CS的不同之处在于,它具有更广泛的心肌损伤和较差的患者预后。然而,患者预后的关键决定因素似乎是心肌损伤的程度,而不是组织病理学诊断。
原始出处:
Hanna‐Kaisa Nordenswan.et al.Manifestations and Outcome of Cardiac Sarcoidosis and Idiopathic Giant Cell Myocarditis by 25‐Year Nationwide Cohorts.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.019415
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心脏结节病#
51
#特发性#
51
#AHA#
60
#巨细胞#
81
学习
100