Sci Transl Med:发现一类独特的免疫细胞促进多发性硬化症产生
2012-08-07 ZinFingerNase 生物谷
来自美国国家卫生研究院的研究人员发现一种独特类型的免疫细胞促进多发性硬化症(multiple sclerosis, MS)产生。他们的发现有助于确定研究作为最新药物之一的达利珠单抗(daclizumab)的疗效,而且还可能导致人们开发出一类新药来治疗多发性硬化症和其他自身免疫疾病。在这些疾病中,免疫系统攻击身体自己的组织。正在进行的临床试验已证实达利珠单抗似乎有助于压制多发性硬化症病人的自身免疫反
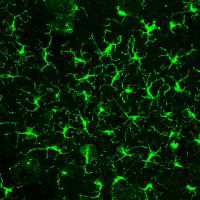
来自美国国家卫生研究院的研究人员发现一种独特类型的免疫细胞促进多发性硬化症(multiple sclerosis, MS)产生。他们的发现有助于确定研究作为最新药物之一的达利珠单抗(daclizumab)的疗效,而且还可能导致人们开发出一类新药来治疗多发性硬化症和其他自身免疫疾病。在这些疾病中,免疫系统攻击身体自己的组织。正在进行的临床试验已证实达利珠单抗似乎有助于压制多发性硬化症病人的自身免疫反应,但是它对组成免疫系统的大批量免疫细胞的精确影响仍然尚未充分理解。
根据这项于2012年8月1日在线发表在Science Translational Medicine期刊上的新研究,研究人员发现达利珠单抗的一种影响就是降低淋巴组织诱导细胞(lymphoid tissue inducer cell, LTi)的数量。已知在胎儿期间,这些细胞促进淋巴结和相关组织的发育,但是它们在成年时的作用仍然是个谜。这项新研究是第一次证实LTi细胞参与任何一种人自身免疫疾病的产生。
论文通信作者Bibiana Bielekova博士和她的研究团队发现在参与临床试验的多发性硬化症病人当中,没有接受达利珠单抗治疗的病人体内LTi细胞的数量比服用这种药物的病人体内的要高。对接受达利珠单抗治疗的病人而言,他们脑脊髓液中的炎症症状减轻。此外,研究人员发现达利珠单抗似乎阻止身体产生LTi细胞,并促进另一种对抗自身免疫反应的细胞类型产生。
在这项新研究中,Bielekova博士和她的研究团队发现达利珠单抗对自然杀伤细胞的促进效应是与它对LTi细胞的抑制效应同时存在的。他们发现这种药物通过它对IL-2信号的影响,作用于一类干细胞。该药物似乎降低这种干细胞产生LTi细胞而让它变成自然杀伤细胞的可能性。
研究人员解释道,达利珠单抗通过抑制LTi细胞,应当能够降低淋巴滤泡的生长。因为科学家们不可能在活的大脑组织中可视化观察这些淋巴滤泡,所以研究人员测量这种药物对脑脊髓液中炎症标记物的影响。他们发现在服用这种药物6.5个月的临床试验病人体内,一种与淋巴生长相关联的蛋白CXCL13和一种用来测量抗体产生的指标IgG指数(IgG index)分别平均下降了50.4%和13.5%。
不过Bielekova提醒道,这些数据只是表明LTi细胞与多发性硬化症病人大脑中的炎症之间存在间接联系。如果进一步研究证实这些细胞在多发性硬化症和其他自身免疫疾病中发挥着重要作用,那么寻求开发新的药物来选择性地抑制LTi细胞可能是一种非常有用的治疗策略。
本文编译自Researchers implicate unique cell type in multiple sclerosis

doi: 10.1126/scitranslmed.3004140
PMC:
PMID:
Inhibition of LTi cell development by CD25 blockade is associated with decreased intrathecal inflammation in multiple sclerosis
Justin S. A. Perry1,*, Sungpil Han1,2,*, Quangang Xu1,3, Matthew L. Herman1, Lucy B. Kennedy1, Gyorgy Csako4 and Bibiana Bielekova
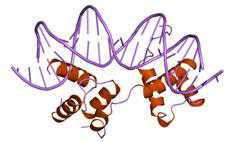
Genetic polymorphisms in the interleukin-2 receptor α (IL-2Rα) chain (CD25) locus are associated with several human autoimmune diseases, including multiple sclerosis (MS). Blockade of CD25 by the humanized monoclonal antibody daclizumab decreases MS-associated inflammation but has surprisingly limited direct inhibitory effects on activated T cells. The present study describes unexpected effects of daclizumab therapy on innate lymphoid cells (ILCs). The number of circulating retinoic acid receptor–related orphan receptor γt–positive ILCs, which include lymphoid tissue inducer (LTi) cells, was found to be elevated in untreated MS patients compared to healthy subjects. Daclizumab therapy not only decreased numbers of ILCs but also modified their phenotype away from LTi cells and toward a natural killer (NK) cell lineage. Mechanistic studies indicated that daclizumab inhibited differentiation of LTi cells from CD34+ hematopoietic progenitor cells or c-kit+ ILCs indirectly, steering their differentiation toward immunoregulatory CD56bright NK cells through enhanced intermediate-affinity IL-2 signaling. Because adult LTi cells may retain lymphoid tissue–inducing capacity or stimulate adaptive immune responses, we indirectly measured intrathecal inflammation in daclizumab-treated MS patients by quantifying the cerebrospinal fluid chemokine (C-X-C motif) ligand 13 and immunoglobulin G index. Both of these inflammatory biomarkers were inhibited by daclizumab treatment. Our study indicates that ILCs are involved in the regulation of adaptive immune responses, and their role in human autoimmunity should be investigated further, including their potential as therapeutic targets.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#硬化症#
64
#TRA#
64
#Transl#
64
#多发性#
50
#Med#
0