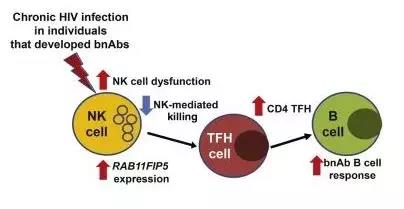
治疗艾滋病,ViiV Healthcare公司的长效注射药物2期临床数据振奋人心
2018-10-31 MedSci MedSci原创
根据临床2期试验LATTE-2的长期数据显示,每八周或每四周注射一次cabotegravir和rilpivirine,显示出"病毒学应答率高,良好的长期耐久性和总体耐受性"。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ALT#
110
#临床数据#
106
学习
147
#2期临床#
123
#HCA#
104
学习了,学习了,学习了
174
#Health#
113