Mol Immunol:外泌体长非编码RNA GAS5能够抑制Th1分化和促进Th2分化
2020-01-06 AlexYang MedSci原创
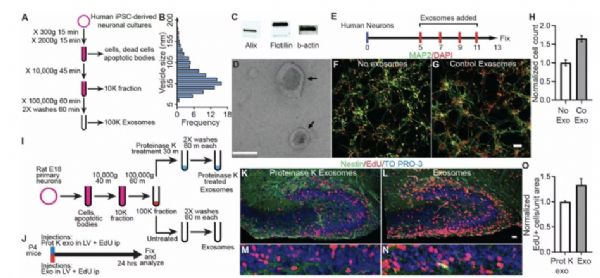
辅助T细胞(Th)1/2分化的不平衡参与了过敏性鼻炎(AR)的发展。最近的研究阐释了外泌体对Th1/Th2分化的调控功能。然而,外泌体中调节上述响应的关键调节因子仍旧不清楚。最近,有研究人员从AR患者的鼻粘液(AR-EXO)和卵清蛋白(OVA)刺激的鼻上皮细胞(OVVA-EXO)中分离了外泌体,并检测了长非编码RNA GAS5(LncGAS5)的表达。结果表明了LncGAS5在AR上皮样本、AR-
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#非编码#
56
#GAS#
49
#长非编码RNA#
50
#编码#
46