Prostate:预后营养指数预测RALP治疗后患者的生化复发
2021-12-11 AlexYang MedSci原创
评价了预后营养指数(PNI)在预测机器人辅助腹腔镜前列腺根治术(RALP)患者生化复发(BCR)中的作用。
最新数据显示,前列腺癌(PCa)是男性第二大最常见的恶性肿瘤,也是第六大死亡原因。根据患者的健康状况,可以推荐积极监测、根治性前列腺切除术(RP)、放疗和化疗等治疗方法。尽管近有30%的患者在手术后出现生化复发,但目前RP仍是治疗局部PCa的最佳选择。已经证明一些临床和病理因素是预测RP术后生化复发(BCR)的独立因素,如肿瘤大小、血管侵犯和手术或穿刺获得的其他结果,但仍然存在侵入性风险和局限性。因此,有必要寻找新的预后参数来帮助预测RP后的临床结果。

近期,来自中南大学湘雅三医院的研究人员在《Prostate》上发表文章,评价了预后营养指数(PNI)在预测机器人辅助腹腔镜前列腺根治术(RALP)患者生化复发(BCR)中的作用。
研究为回顾性分析,参与者为中南大学湘雅三医院泌尿外科的136例接受RALP治疗患者的临床资料。时间为2015年10月到2021年4月。根据临床检查、骨扫描、计算机断层扫描和/或盆腔磁共振成像的结果确定了临床分期。通过针刺活检和病理组织学检查确诊PCa。观察的终点是BCR。评估了接收者操作特征(ROC)曲线下面积,确定了PNI的最佳截断值。使用了Kaplan-Meier分析和Cox比例风险模型评估了PNI与BCR的相关性。
136名行RALP患者的中位年龄为68岁。基线PSA水平中位数为15.39纳克/毫升。其中,26名患者(19.1%)有淋巴结转移,77名患者(56.6%)有阳性手术边缘。此外,67名患者(49.3%)有神经侵犯,46名患者(33.8%)的Gleason评分在8至10之间。T3和T4之间的临床分期的患者占50.7%。术前PNI中位数为48.73。根据ROC曲线,PNI的最佳截断值为46.03(95%置信区间:0.604-0.805,尤登指数=0.401,敏感性=82.5%,特异性=57.6%,P<0.01)。多变量Cox分析显示,临床分期、前列腺特异性抗原和PNI是预测RALP治疗患者BCR的独立预后因素。
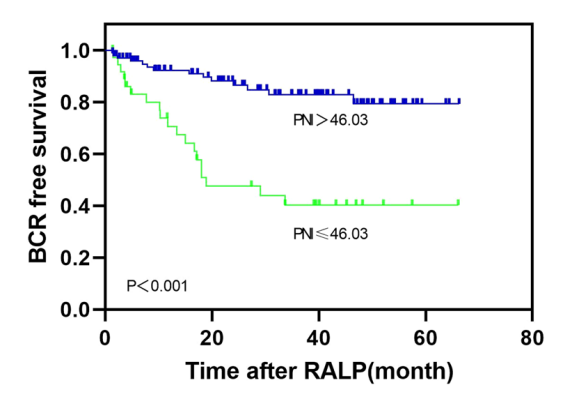
根据PNI值的RALP后无BCR生存情况
综上所述,PNI是预测RALP治疗患者BCR的一个独立预后因素。因而将PNI纳入风险评估可提供更多的预后信息。
原始出处:
Nichujie Li , Wei-Jie Song , Jun Gao et al. The prognostic nutritional index predicts the biochemical recurrence of patients treated with robot-assisted laparoscopic radical prostatectomy. Prostate. Nov 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ALP#
139
#ROS#
86
#生化复发#
106
#PRO#
91