Blood:抗凝药物不能阻断组织因子和血小板触发的静脉血栓形成
2019-03-23 不详 MedSci原创
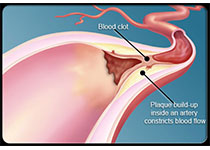
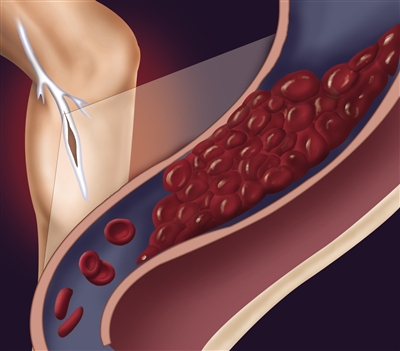
中心点:抗凝血酶和C蛋白被抑制后,组织因子和血小板是小鼠静脉血栓形成的限速因子。在本动物模型中,凝血因子XII和循环中的中性粒细胞不限制静脉血栓形成的速度。摘要:组织因子、凝血因子XII、血小板和中性粒细胞在静脉血栓形成(VT)的病理生理过程中具有重要作用。在需要手术处理才能诱发VT的小鼠模型中,它们的作用变得很明显。在小鼠中,仅采用小干扰RNA(siRNA)联合抑制天然抗凝血剂抗凝血酶(Serp
抗凝血酶和C蛋白被抑制后,组织因子和血小板是小鼠静脉血栓形成的限速因子。
在本动物模型中,凝血因子XII和循环中的中性粒细胞不限制静脉血栓形成的速度。
摘要:
组织因子、凝血因子XII、血小板和中性粒细胞在静脉血栓形成(VT)的病理生理过程中具有重要作用。在需要手术处理才能诱发VT的小鼠模型中,它们的作用变得很明显。在小鼠中,仅采用小干扰RNA(siRNA)联合抑制天然抗凝血剂抗凝血酶(Serpinc1)和蛋白C (Proc)也可导致静脉血栓形成表型,最明显的是头部大静脉血管阻塞。VT可致死,但通过抑制凝血酶可完全挽救。
在本研究中,研究人员采用VT小鼠模型来研究组织因子、凝血因子XII、血小板和中性粒细胞在静脉血栓形成过程中的作用。
总而言之,凝血酶和蛋白C被抑制后,静脉血栓形成依赖于组织因子和血小板,而不依赖于凝血因子XII和循环中性粒细胞。本研究表明在小鼠静脉血栓形成的过程中,不同的促凝通路在发挥作用,依赖于触发刺激。
Marco Heestermans, et al.Mouse venous thrombosis upon silencing of anticoagulants depends on tissue factor and platelets, not FXII or neutrophils.Blood 2019 :blood-2018-06-853762; doi: https://doi.org/10.1182/blood-2018-06-853762
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉血#
76
#阻断#
71
#静脉#
72
#组织因子#
97
#静脉血栓形成#
83