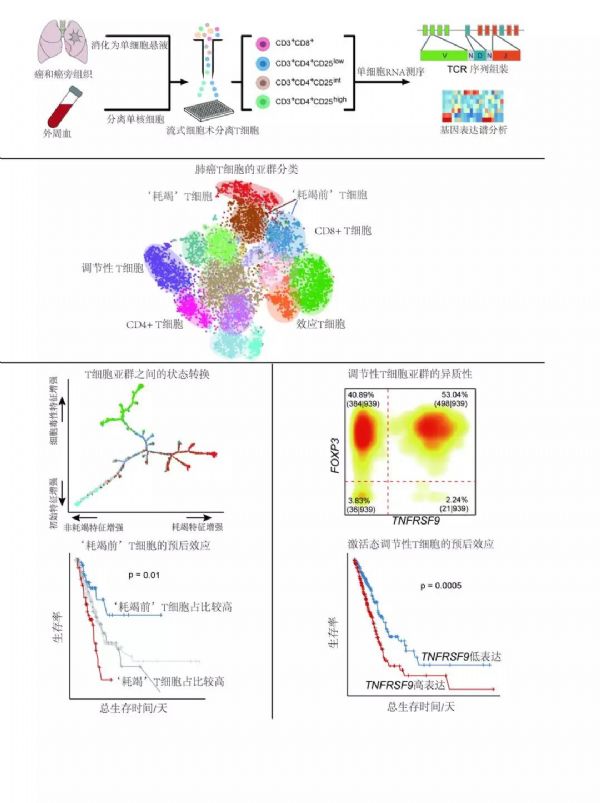
Nat Med:张泽民研究组与合作者发表单细胞水平的肺癌 T 淋巴细胞免疫图谱
2018-06-27 佚名 生物360
肺癌被称为“癌中之王”,其发病率和致死率在所有癌症中均居首位,其中 85% 的肺癌属于非小细胞肺癌。考虑到肿瘤微环境的复杂性,近年来单细胞转录组测序技术逐渐被广泛应用于肿瘤浸润免疫细胞的研究当中。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
110
学习了.谢谢作者分享!
113
#淋巴细胞#
67
#细胞免疫#
76
#Med#
74
好
105
学习了.谢谢分享
90
个个都宣称是癌中之王!谢谢分享最新科研成果!
98
学习
132
不错的文章值得拥有哦!
71