NEJM:眼睑部位出现持续性红斑和瘙痒病例报道
2015-12-31 MedSci MedSci原创
http://www.nejm.org/doi/full/10.1056/NEJMicm1501675
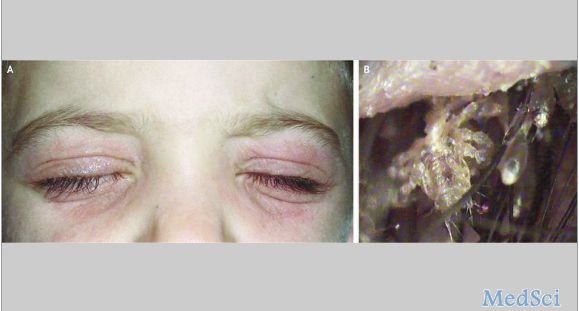
男性,6岁,因眼脸部位出现持续性红斑和瘙痒而来源就诊(如图A所示)。
据了解,该男孩在来源之前曾在当地医院就诊,会诊医师诊断为特应性皮炎并应用糖皮质激素外用和抗组胺药进行治疗但疗效并不明显。
皮肤镜检查发现,在该男孩的眼睫毛上可见几个阴虱在活动并发现有虫卵(如图B和视频所示)。
最后,会诊医师确诊该男孩所患为眼睑阴虱病。
随后,该男孩遵医嘱5%黄降汞软膏外涂,每日四次,持续用药2周后症状完全消失。
在本案例中,该男孩眼脸睫毛处的环境,类似于成年人的会阴部,因此容易导致阴虱在此处繁殖。而感染者一般都是通过与受感染者的密切接触传播的。
由于眼脸阴虱在肉眼下难以发现,通常只能通过皮肤镜检查才可识别,因此,在临床上阴虱病经常被误诊为过敏性皮炎或过敏性结膜炎。
原始出处:
Micali G, Lacarrubba F.Phthiriasis Palpebrarum in a Child. N Engl J Med. 2015 Dec 31;373(27):e35.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#眼睑#
0
好,值得学习
134
#持续性#
51
是一篇不错的文章
118
值得进一步关注
88
不错,赞一个
101
这篇文章有一定深度
51
少见
78
多排查
88
这个少见
135