Cell Stem Cell:常被人忽视的脉络丛竟能调控大脑中的神经干细胞
2016-07-23 佚名 生物谷
在一项新的研究中,来自瑞士巴塞尔大学生物中心的Fiona Doetsch教授团队发现作为大脑中很大程度上被忽视的产生脑脊髓液的结构,脉络丛(choroid plexus)在调节成体神经干细胞中发挥重要的作用。这项研究也证实脉络丛分泌的信号在影响干细胞行为的衰老期间发生动态变化。相关研究结果于2016年7月21日在线发表在Cell Stem Cell期刊上,论文标题为“Age-Dependent N
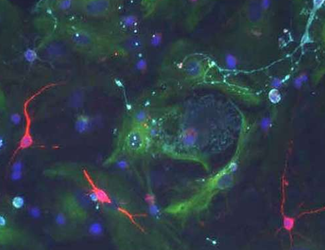
在一项新的研究中,来自瑞士巴塞尔大学生物中心的Fiona Doetsch教授团队发现作为大脑中很大程度上被忽视的产生脑脊髓液的结构,脉络丛(choroid plexus)在调节成体神经干细胞中发挥重要的作用。这项研究也证实脉络丛分泌的信号在影响干细胞行为的衰老期间发生动态变化。相关研究结果于2016年7月21日在线发表在Cell Stem Cell期刊上,论文标题为“Age-Dependent Niche Signals from the Choroid Plexus Regulate Adult Neural Stem Cells”。
干细胞是在不同器官中发现的非特化细胞。它们能够分化为体内的特化细胞。在成年大脑中,神经干细胞在一生当中产生神经元。它们位于独特的微环境中,其中这种微环境提供关键的信号来调节干细胞自我更新和分化。
成年大脑中的神经干细胞接触脑室,即充满着脑脊髓液的腔室。脑脊髓液是由脉络丛产生的。在这项新的研究中,研究人员证实脉络丛是神经干细胞微环境的一个关键组分,并且它的性质在一生当中会发生变化并且影响神经干细胞的行为。
脉络丛信号调节神经干细胞
Doetsch团队发现脉络丛分泌脑脊髓液中众多重要的信号因子,这些信号因子在一生当中调节神经干细胞中发挥着重要作用。在衰老期间,神经干细胞分裂水平和新的神经元形成数量下降。该团队证实尽管神经干细胞仍然存在于衰老的大脑中,也能够分裂,但是它们更少这样做。论文第一作者Violeta Silva Vargas解释道,“一种原因就是在老化的脉络丛中的信号是不同的。因此,神经干细胞在衰老期间接受到不同的信息,更不能够形成新的神经元。换言之,破坏神经干细胞在这个大脑区域中的健康状态。但是真正令人惊讶的是,当将衰老的神经干细胞与来自年轻的脊髓液中的信号一起培育时,它们仍然能够经激活后进行分裂---表现得象年轻的神经干细胞那样。”
理解健康状态和患病状态下大脑功能的新途径
在未来,Doetsch团队计划研究脉络丛分泌的信号因子组成和不同状态下的这些变化如何影响神经干细胞。这可能为改变健康状态和患病状态下的大脑功能提供新的途径。Doetsch说,“我们的研究也为理解人体不同生理状态如何影响健康状态和患病状态下大脑中的神经干细胞开辟新方向,而且也为开发新疗法提供新的思路。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
80
#脉络丛#
107
#stem cell#
96
#Cell#
65
#STEM#
80
#神经干细胞#
71