Chest:非囊性纤维化支气管扩张的药物治疗!
2017-05-12 xing.T MedSci原创
在两个支气管扩张患者的全国性的样本中ICS的使用是很常见的,相对较少的患者接受了抑制性抗生素治疗。需要进一步的研究以明确这些疗法在支气管扩张症患者的安全性和有效性。
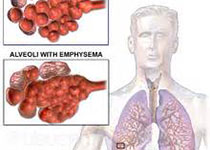
非囊性纤维化支气管扩张(“支气管扩张症”)是一种慢性炎症性肺疾病常与非结核分枝杆菌(NTM)感染有关。很少有数据指导支气管扩张的治疗决策。近日,胸部疾病领域权威杂志Chest杂志上发表了一篇研究文章,研究人员试图描述美国吸入性糖皮质激素(ICS)和抗生素治疗的模式。
研究人员通过NTM信息研究(NTMir)邀请了2000例患者完成匿名电子问卷调查。研究人员分别对来自于美国支气管扩张及NTM注册研究(BRR)的基础临床和实验室数据进行分析。
在511例NTMir调查反馈的支气管扩张患者中,平均年龄为67岁,85例(17%)报告了哮喘,99例(19%)报告了慢性阻塞性肺疾病(COPD)。有282例(55%)参与者报告使用了ICS治疗,其中有171例(61%)治疗超过1年以及150例(53%)目前正在进行ICS治疗。很少有报道曾以阿奇霉素治疗非NTM支气管扩张(203例,40%)或吸入妥布霉素(78例,15%)。1912例BRR患者的中位年龄为69岁,528例(28%)有哮喘,360例(19%)有慢性阻塞性肺疾病。在740例无NTM的患者中,314例(42%)患者在研究之初接受了ICS治疗。在接受ICS治疗的非NTM患者中,只有178例(57%)患者有COPD或哮喘的合并诊断,从而可以解释ICS使用。较少的受试者服用抑制性大环内酯类抗生素(96例,13%)、70例(10%)服用吸入抑制性抗生素,48例(68%)患者有铜绿假单胞菌感染。
在两个支气管扩张患者的全国性的样本中ICS的使用是很常见的,相对较少的患者接受了抑制性抗生素治疗。需要进一步的研究以明确这些疗法在支气管扩张症患者的安全性和有效性。
原始出处:
E. Henkle; T.R. Aksamit, et al. Pharmacotherapy for non-cystic fibrosis bronchiectasis: results from an NTM Info & Research patient survey and the Bronchiectasis and NTM Research Registry.Chest. 2017. http://journal.publications.chestnet.org/article.aspx?articleid=2627077
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Chest#
0
#扩张#
72
#支气管#
68
#EST#
64
#非囊性纤维化支气管扩张#
74
#囊性#
80
提高了自己,认真学习
106
学习了谢谢分享
96