Alzheimers Dement:种族不同,阿尔兹海默相关指标的长期变化趋势不同
2022-03-08 Freeman MedSci原创
该研究的重要意义在于观察到淀粉样蛋白生物标志物的纵向种族差异。
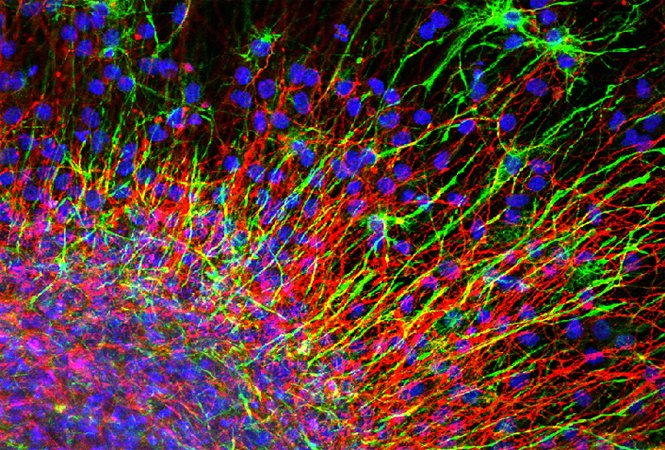
阿尔茨海默病(AD)是一种不可逆的神经退行性疾病,影响到600万美国人,预计到2050年病例将增加一倍以上。在没有真正有效的治疗方法可以改变AD的进展的情况下,预防可能是唯一可行的选择,可以控制公共健康危机。
 为了设计AD的预防试验,生物标志物对于建立适当的纳入/排除标准和跟踪疾病进展非常重要。 几十年的生物标志物研究已经确定了一系列AD生物标志物的有效性,以检测大脑中的淀粉样β(Aβ)和神经纤维缠结(NFTs),以及相关的神经元死亡和神经退化。包括使用[11C]苯并噻唑示踪剂、匹兹堡化合物B(PiB)和其他示踪剂(18F-AV45)、脑脊液(CSF)分析物、Tau PET区域摄取量和基于磁共振成像(MRI)的大脑结构测量,利用正电子发射断层扫描(PET)对大脑纤维状Aβ进行分子成像。
为了设计AD的预防试验,生物标志物对于建立适当的纳入/排除标准和跟踪疾病进展非常重要。 几十年的生物标志物研究已经确定了一系列AD生物标志物的有效性,以检测大脑中的淀粉样β(Aβ)和神经纤维缠结(NFTs),以及相关的神经元死亡和神经退化。包括使用[11C]苯并噻唑示踪剂、匹兹堡化合物B(PiB)和其他示踪剂(18F-AV45)、脑脊液(CSF)分析物、Tau PET区域摄取量和基于磁共振成像(MRI)的大脑结构测量,利用正电子发射断层扫描(PET)对大脑纤维状Aβ进行分子成像。
这些研究进一步表明,AD的神经病理过程在症状出现前几年甚至几十年就开始了,生物标志物的变化遵循一个时间序列,早期Aβ在大脑中积累和沉积,随后形成NFTs、神经元死亡和大脑结构变化。
然而,几乎所有这些重要的发现都是基于以白人为主的队列,少数报告AD生物标志物变化种族差异的生物标志物研究都是基于横断面数据。
藉此,华盛顿大学的Chengjie Xiong等人,评估黑人和白人在所有主要AD生物标志物中的纵向差异,包括CSF、淀粉样PET和结构MRI。

共有179名黑人和1180名白人在基线时认知正常,并有至少一种生物标志物模式的纵向数据,对他们的年度变化率进行分析。
他们发现:黑人的CSF淀粉样β(Aβ)42/Aβ40下降得更慢(P=0.0390),淀粉样蛋白(PET)积累得更慢(P=0.0157)。
黑人和白人的CSF Aβ42随时间变化的方向相反(P = .0039)。
黑人的CSF总tau和磷酸化tau181的年增长率约为白人的一半。
该研究的重要意义在于观察到淀粉样蛋白生物标志物的纵向种族差异。全面和前瞻性地研究ApoE基因型和社会文化因素对这些差异的影响将是很重要的。
原文出处:
Xiong C, Luo J, Schindler SE, Fagan AM, Benzinger T, Hassenstab J, Balls-Berry JE, Agboola F, Grant E, Moulder KL, Morris JC. Racial differences in longitudinal Alzheimer's disease biomarkers among cognitively normal adults. Alzheimers Dement. 2022 Feb 25. doi: 10.1002/alz.12608. Epub ahead of print. PMID: 35218143.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#alzheimers#
107
#ERS#
85
#长期变化#
81
#MERS#
87
#阿尔兹海默#
118