Clinical Gastroenterology H: 慢性炎症性肠病活动的Nancy指数评分与大肠肿瘤发病相关
2019-12-27 不详 MedSci原创
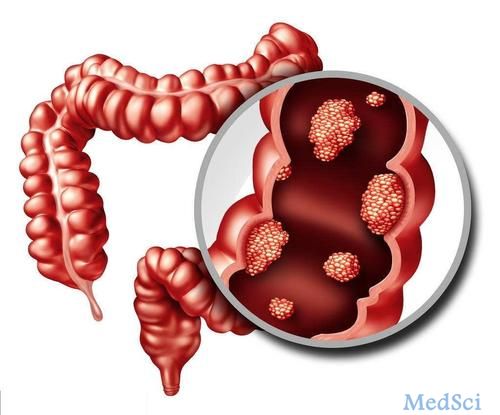
组织学和内镜下疾病活动的程度与炎性肠病(IBDs)患者大肠肿瘤形成(CRN)的风险增加相关,但是尚无任何组织学评分系统可用于确定CRN的风险。本项研究调查了存在组织学和内镜下疾病活动的IBD患者与CRN风险之间的关联。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#AST#
65
#Gastroenterol#
46
#GAS#
51
#Gastroenterology#
44
#clinical#
53
#炎症性#
49