Neurology:反复撞击致慢性创伤性脑病后,FLAIR白质高信号与神经病理、认知改变之间的关系
2021-12-08 Naomi MedSci原创
运动导致的反复头部撞击与神经退行性疾病慢性创伤性脑病(CTE)有关。WMH可能捕捉到重复性头部撞击的长期白质病变,除微血管疾病外,还包括白质稀疏和β-tau病变。需要进行前瞻性的影像-病理相关性研究。
运动导致的反复头部撞击以及由此导致的症状性脑震荡和无症状亚临床脑震荡与神经退行性疾病慢性创伤性脑病(CTE)有关。慢性创伤性脑病的病理性损害包括脑沟深处神经元中过度磷酸化的tau(p-tau)的血管周围聚集体,有或没有星形胶质细胞。CTE的临床表现可包括认知能力下降和神经行为调节障碍。不是所有的症状都与p-tau有关。
尸检研究表明,脑白质变性和微血管损伤是反复头部撞击的晚期病理特征,这些都会导致神经认知障碍。FLAIR MRI序列上的白质高信号(WMH)可能是研究重复头部撞击对白质的晚期影响的有效工具。白质高信号的病因是多因素的,但通常被解释为血管危险因素(VRF)引起的脑小血管疾病的标志。WMH也可以反映阿尔茨海默病(AD)神经病理变化的轴突变性,并且是冠状的。有研究在86名有症状的前国家橄榄球联盟(NFL)球员中发现,T1白质低强度与更多反复头部撞击有关,控制了VRF。白质低强度越大,执行功能越差。
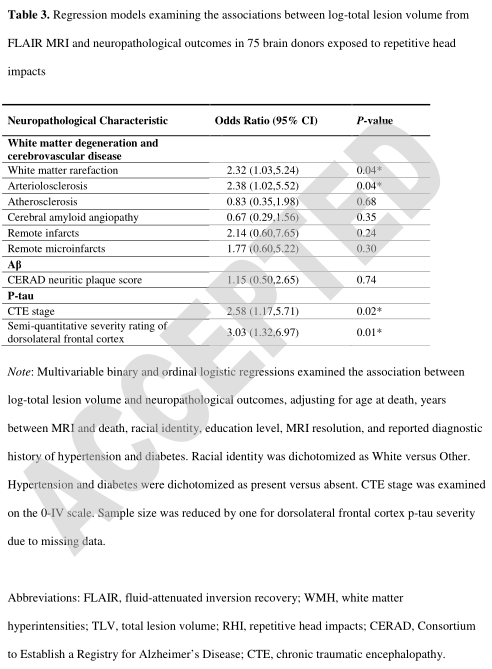
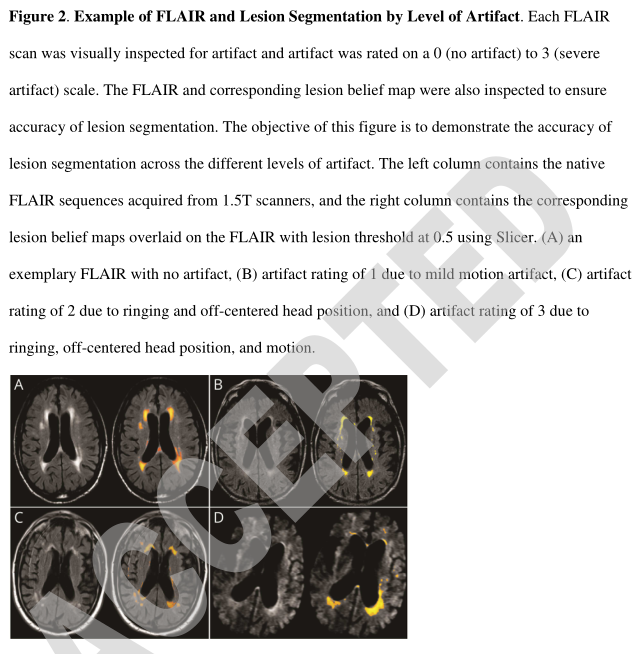
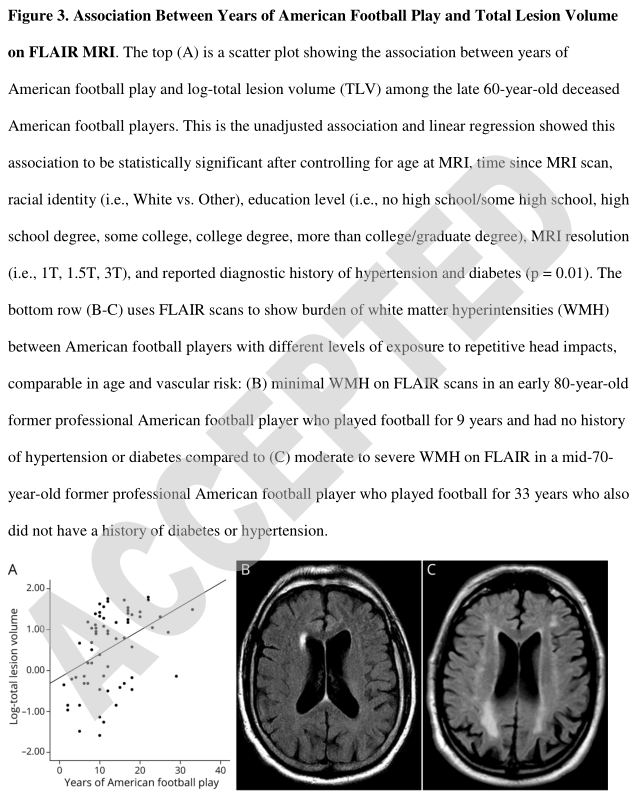
辨别FLAIR WMH在反复头部撞击人群中是否有独特的危险因素和潜在的病理改变需要进行影像-病理相关性研究。在反复头部撞击的脑供者中,近日,有研究人员研究了生前FLAIR WMH与 (1)白质稀疏、动脉硬化、动脉粥样硬化、脑淀粉样血管病的神经病理分级、CERAD Aβ神经斑块评分、p-tau严重程度以及是否存在远隔梗死灶、微梗死灶和微出血的关系;(2)参加美式橄榄球比赛的年限(重复头部撞击暴露的指标);以及(3)回顾性信息。
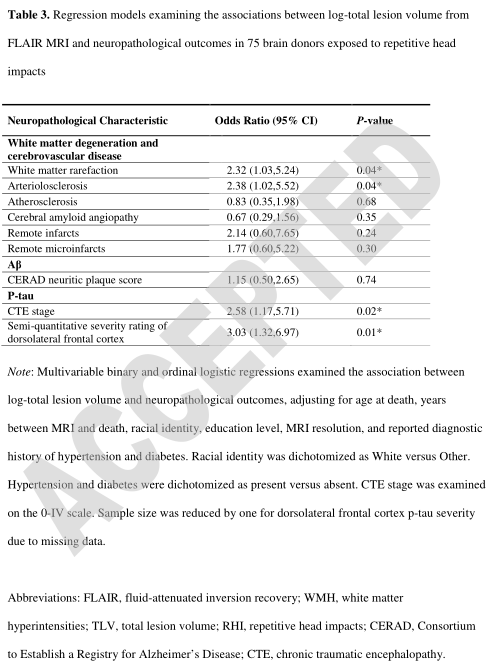
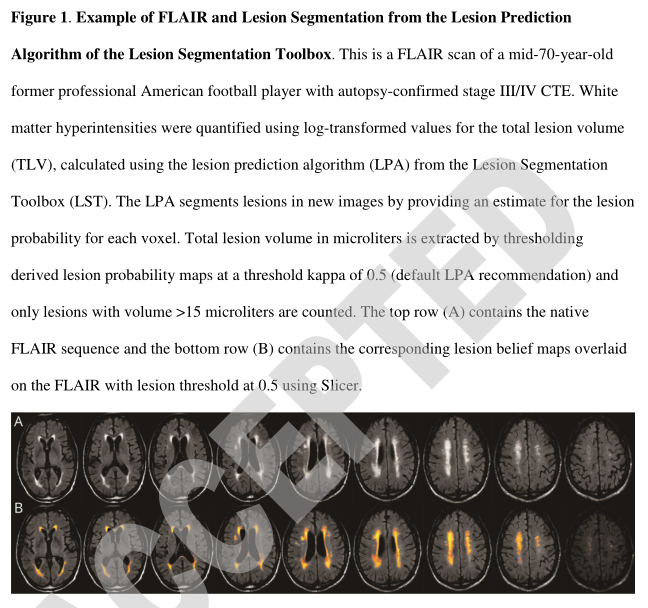
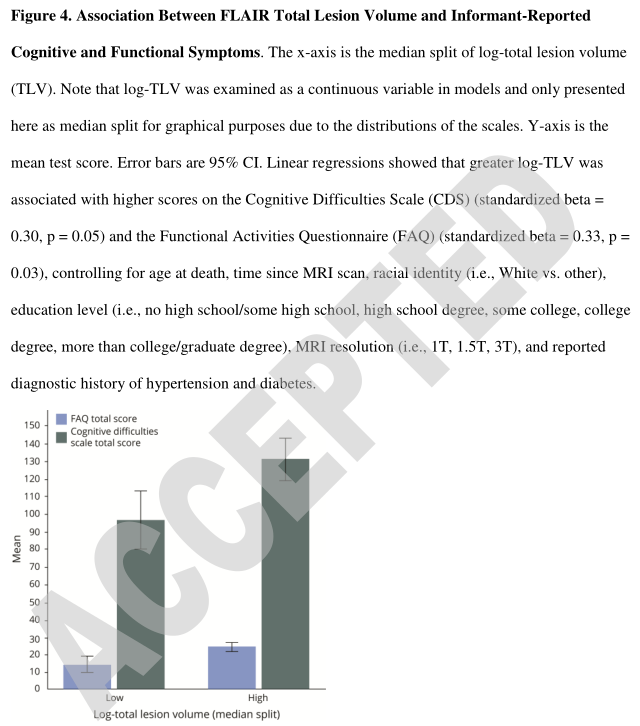
这项影像-病理相关性研究包括反复头部撞击的有症状的已故男性。捐献者从病历中进行了生前FRAIR扫描,没有发现中枢神经系统肿瘤、大血管梗死、出血和/或脑软化症的证据。用病变总体积(TLV)的对数转换值来量化WMH,该值使用病变分割工具箱中的病变预测算法计算。神经病理学评估包括白质稀疏、脑血管疾病、p-tau严重程度(CTE期、额叶背外侧)和Aβ的半定量分级。在足球运动员中,踢球年限是重复头部撞击暴露的指标。回溯采用认知困难量表(CDS)和功能活动问卷(FAQ)评定被调查者报告的认知功能和日常生活功能。控制人口统计学、糖尿病、高血压和MRI分辨率的回归模型。统计学意义定义为p<0.05。
- 样本包括75名捐献者:67名足球运动员和8名非足球接触运动运动员和(或)退伍军人。痴呆是最常见的MRI指征(64%)。
- 尸检时有53例(70.7%)有CTE。
- LOG-TLV与白质稀疏(OR=2.32,95%CI=1.03,5.24,p=0.04)、动脉硬化(OR=2.38,95%CI=1.02,5.52,p=0.04)、CTE分期(OR=2.58,95%CI=1.17,5.71,p=0.02)、额叶背外侧病变严重程度(OR=3.03,95%CI=1.32,6.97,p=0.01)相关,与Aβ无关。
- 踢球年限与LOG-TLV相关(b=0.04,95%CI=0.01,0.06,p=0.01)。
- 较大的LOG-TLV与较高的FAQ(非标准化β=4.94,95%CI=0.42,8.57,p=0.03)和CDS得分(非标准化β=15.35,95%CI=-0.27,30.97,p=0.05)相关。
WMH可能捕捉到重复性头部撞击的长期白质病变,除了微血管疾病外,还包括白质稀疏和β-tau病变。需要进行前瞻性的影像-病理相关性研究。
这项研究提供了四类证据,证明了FLAIR白质高信号与神经病变(白质稀疏、动脉硬化、β-tau堆积)、多年的美式橄榄球比赛以及报告的反复头部撞击下有症状的脑捐赠者的认知症状之间的关系。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#创伤性#
111
#白质#
95
#高信号#
82
#脑病#
101
#慢性创伤性脑病#
82
学习
79
好文
85
学习
95
#Neurol#
76
#创伤#
78