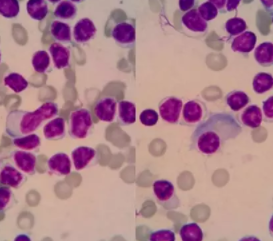
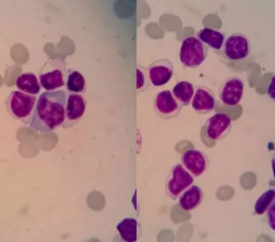
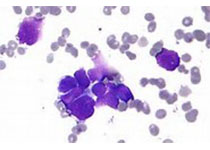
病例分享:淋巴浆细胞淋巴瘤/华氏巨球蛋白血症?一例分析
2017-12-06 承德医学院附属医院检验科 杨新宏 检验视界网
患者男,68岁,主因:左侧胸痛5个月,呼吸困难半个月入院。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#淋巴浆细胞淋巴瘤#
55
#球蛋白#
42
#细胞淋巴瘤#
46
#浆细胞#
39
诊断详细.思路清晰
82
学习一下谢谢分享
77
好全
91
学了........
97
学习一下谢谢
78