【一般资料】
患者,38岁
【主诉】
因孤立性纤维瘤术后2年,随访超声检查发现右侧附件区肿物,于2013年3月11日入院诊治。
【现病史】
患者曾于2011年4月,因自诉尿频、尿急3个月,左下腹痛1个月,弯腰时有压迫感于我院就诊,彩超检查提示:盆腔左侧实性肿物,内为等回声光团,大小约70mm×64mm×54mm。血清肿瘤标志物CEA、AFP、CA125均正常。术前诊断为“盆腔包块性质待查”。行剖腹探查术,术中见:子宫居中,常大,双侧附件正常,腹膜后左髂窝内70mm×60mm×60mm肿物,故行“阔韧带肿物切除术”。术中冰冻病理检查提示:梭形细胞肿瘤,部分区域细胞密集,生长活跃。免疫组化:CD34(+)、Vimentin(+)、Atin(+)、HMB45弱(+)、CD117(+)、CK(-)、S100(-)。术后病理诊断为阔韧带间质瘤。解放军总医院(北京301医院)会诊诊断“孤立性纤维瘤”。患者术后未行进一步治疗,定期随诊。此次随诊彩超检查提示:右侧附件区包块36mm×38mm×32mm,轮廓欠规则,内为不均质低回声,伴带状高回声,CDFI示血流信号较丰富(RI=0.48)。遂于当日收入住院行进一步诊治。
【家族史】
家族史无特殊。
【体格检查】
外阴、阴道正常,宫颈光滑,子宫正常大小,右侧附件区增厚,无压痛,左侧附件区未及异常。
【辅助检查】
CT检查提示:右侧附件区可见椭圆形软组织密度影,边界清楚,动脉期右侧卵巢静脉显影,沿腰大肌下行,进入右侧附件区肿物,约3.9cm×4cm大小,呈明显血管样强化,并与右侧髂动脉分支相交通,可见分隔,局部侧支循环显示呈内网迂曲血管影。
【初步诊断】
右侧附件区占位,血管源性畸形(卵巢动静脉畸形?)与富血供肿瘤鉴别。
【治疗】
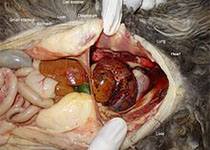
于3月14日行腹腔镜下病灶切除术治疗,术中见盆腔广泛粘连,子宫正常,右前侧壁圆韧带略下方见血运极丰富肿物,直径约3cm,其与子宫和侧腹壁相连续,肿物基底部位于右髂窝内,切除肿物。另于大网膜上见两枚血运极丰富种植样肿物,直径分别为1.5cm及1cm,切除两处病灶。肿物均质地脆、呈鱼肉样,装入取物袋取出,术中冰冻病理检查提示:梭形细胞肿瘤,考虑为间叶来源。术后石蜡病理检查提示:间叶来源肿瘤,部分细胞生长活跃,见异型及病理性核分裂;免疫组化CD34(+)、CD99(+)、CD117(-)、S100(-)、Desmin(-)、Actin(-)、HMB45(-)、CD10(-)、SMA(-)、Ki67约10%,结合其2年前病史,考虑为孤立性纤维瘤复发。术后随访至今再无复发。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了感谢分享
68
#纤维瘤#
64
#孤立性#
58
很好的文章.谢谢分享
87
非常好的文章.学习了
77