腰椎间盘突出症CT报告有椎管狭窄,不一定要治疗狭窄本身
2022-09-02 放射沙龙 健康新语
腰椎间盘突出症造成的间歇性跛行为神经性间歇性跛行,在腰椎间盘突出症康复后,症状基本同步消失,个人建议先按照腰椎间盘突出症处理,大都会获得很好的康复。
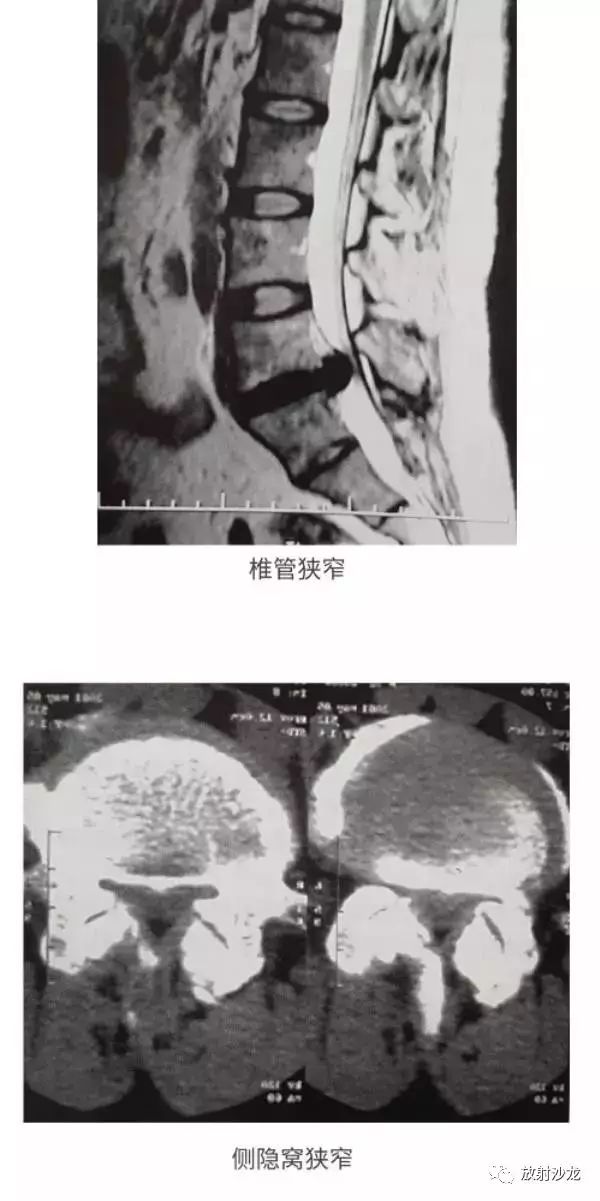
小编在从事康复工作中遇到的不少的腰椎间盘突出症案例,因为先天性椎管直径就比较小或者突出物又相对的较大,突向椎管的方向就引起继发性的中央型椎管狭窄,突向侧隐窝方向也可造成侧隐窝的狭窄,在CT或者核磁的报告中有明确标注。这部分人中有一些人会在行走时,随行走的距离增加,引起腰背痛或不适,同时感觉到有症状的一侧疼痛麻木加重,在蹲下休息或者卧床休息后症状逐渐消失。另一部分人如无间歇性跛行,可不考虑椎管狭窄和侧隐窝狭窄问题,不要因为报告有而苦恼。
造成间歇性跛行的表现不同,主要分为两种常见情况,一种少见特例,我们要通过症状来进一步分析去辨别,而不能单纯的通过跛行就确诊是椎管狭窄引起的,或者急于按照椎管狭窄侧隐窝狭窄治疗,这里我主要讲前两种。

腰椎间盘突出症造成的间歇性跛行为神经性间歇性跛行,在腰椎间盘突出症康复后,症状基本同步消失,一般不需要针对椎管狭窄去考虑手术,它造成的症状主要是由于行走时,椎管内受阻的静脉丛逐渐充血,引起神经根的充血加重或脊髓血管扩张,加重了对神经根的压迫,引起症状加重,主要临床表现为不明确的、多种表现的疼痛(如放射痛、绞痛、沉重感);体现在肢体广泛疼痛感,包括臀部腿部放射痛,从近端放射到远端(从腰到脚),行走后疼痛加重,站立时也会加重;身体前屈时疼痛减轻,一旦疼痛出现,大都需要平卧或坐下缓解疼痛,缓解时间也较长;伴有神经感觉异常,直腿抬高可能出现阳性,可能出现神经损伤,血管存在搏动。个人建议先按照腰椎间盘突出症处理,大都会获得很好的康复。
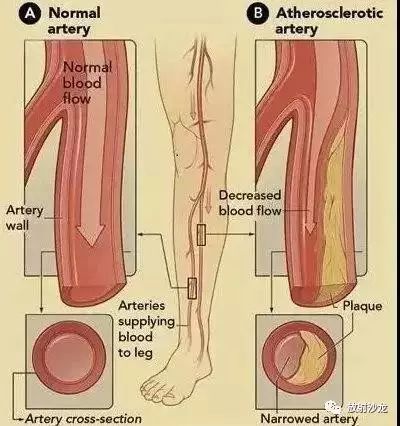
血管性间歇性跛行,主要是下肢动脉闭塞可能出现类似问题,表现为锐痛和绞痛,多位于腓肠肌,极少数位于臀部,出现在大腿的更少几乎不存在,没有放射性疼痛,步行疼痛加重,爬山时更为明显,疼痛时站立不动,停止肌肉活动,疼痛很快的可以缓解,短的时间数秒都可,直腿抬高隐形,无神经损伤,下肢动脉无脉搏搏动,如股动脉、腘动脉搏动消失,基本可以确诊,此问题要早发现早重视,不然有截肢,甚至生命危险。
脊髓源性跛行,可能出现在脊髓内血管病变、动-静脉血管畸形等脊髓内源性问题,也可有胸椎黄韧带骨化、CSM等外源性脊髓压迫。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#椎管狭窄#
114
#椎间盘突出#
97
#椎管#
97
#腰椎#
55
#腰椎间盘#
70