Stroke:D-二聚体水平可提前预测大血管闭塞
2021-02-16 Freeman MedSci原创
D-二聚体水平可提前预测大血管闭塞
血管内治疗(EVT)随机临床试验的荟萃分析和汇总分析一致显示,与最佳医疗治疗相比,大血管闭塞症在卒中后头6小时内的伤残率平均降低2.5倍。根据DAWN(弥散加权成像[DWI]或计算机断层灌注[CTP]评估与临床失配分流清醒和晚期出现的脑卒中进行神经干预)和DEFUSE-3(缺血性脑卒中影像学评估后的血管内治疗)试验结果,6小时以上的EVT实现功能独立的效果更强。由于血管内治疗的可获得性有限,且其疗效具有时间依赖性,因此亟需制定策略,以确定那些患者是EVT的候选者。急性缺血性卒中的大血管闭塞(LVO)诊断对指导治疗决策至关重要,但它高度依赖于先进的神经影像技术,如计算机断层血管造影(CTA),使得院前和社区医院的诊断变得复杂。在这些情况下,转入综合卒中中心主要依据临床评分。
血液生物标志物代表了分子特征的客观测量,已被提出作为帮助急性卒中诊断的工具。
在这样的背景下,循环生物标志物或许可以帮助识别严重的脑卒中(具有较高的藏匿LVO的可能性)。
藉此,西班牙Hospital Universitario Central de Asturias的Anna Ramos-Pachón等人,探究了和卒中量表相关的血液生物标志物是否有助于提高LVO的早期诊断。
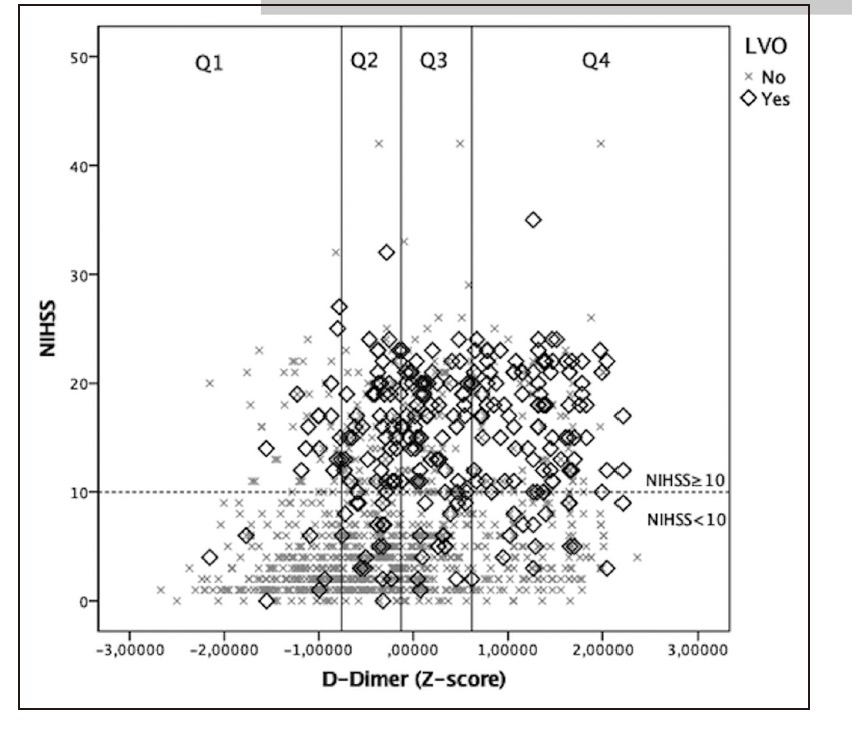
他们基于Stroke-Chip队列,它是在加泰罗尼亚6个卒中中心进行的一项前瞻性观察研究。他们在连续患者出现症状的前6小时内采集血液样本。用NIHSS评估卒中严重程度,评估LVO。使用logistic回归模型评估多种血液生物标志物与LVO的独立关联,并评估了NIHSS以及NIHSS和选定的血清生物标志物水平组合的敏感性、特异性和预测值。
 结果显示:13008例疑似脑卒中患者被纳入,为期17个月。
结果显示:13008例疑似脑卒中患者被纳入,为期17个月。
131名患者未评估LVO。1177名患者纳入进行分析(平均年龄69.3岁,56%为男性,中位基线NIHSS为6,中位采血时间为2.5小时)。262名患者中检测出LVO。LVO患者年龄较大,基线NIHSS较高,有房颤病史,从卒中发病到入院时间较短。经过logistic回归分析,D-二聚体仍然是LVO的独立预测因子(OR=1.59)。
和单独使用NIHSS的模型相比,纳入了D-二聚体水平和NIHSS评分对检测LVO,表现出更好的特异性和阳性预测价值。
这个研究的重要意义在于,发现了早期D-二聚体水平是LVO的独立预测指标,可能有助于更好地筛查院前患者,并转运至合适的卒中中心接受合适的治疗。
原文出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管闭塞#
104
#二聚体#
112
#大血管#
102
学习了,受益了!
106
#D-二聚体#
137
学习了#D二聚体#
179
D二聚体临床上很有意义
110