Blood:SHP2功能异常通过影响血小板的信号和功能导致努南综合征
2019-10-02 MedSci MedSci原创
SHP2,由PTPN11基因编码,是一种普遍存在的蛋白酪氨酸磷酸酶,是信号转导的关键调节因子。PTPN11基因的胚系突变导致SHP2的催化功能获得或丧失,分别可导致两种多器官缺陷的疾病:Noonan综合征(NS)和伴随多发雀斑的NS(NSML)。NS患者常发生出血异常,但病因尚不明确。本研究在NS/NSML患者中和携带导致这两种疾病的PTPN11突变的两种小鼠模型中研究血小板激活。NS小鼠和患者来
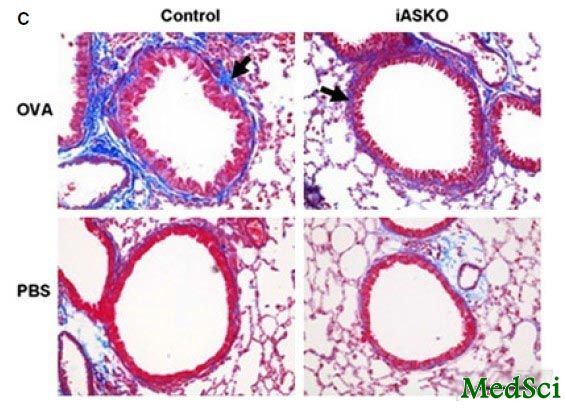
NS小鼠和患者来源的血小板在低浓度GPVI和CLEC-2激动剂的诱导下聚集显著减少,而且在动脉剪切应力下胶原表面血栓生长也减少。这与GPVI和aIIbb3整合素信号、血小板分泌和TXA2生成缺陷有关。同样,NS小鼠颈动脉局部损伤后,动脉血栓的形成明显减少,出血时间明显延长。
与此相反,NSML小鼠的血小板,在GPVI和CLEC-2刺激后的活化增强,在剪切应力作用下,胶原基质上的血小板血栓表型增强。NSML患者来源的血液样本也显示出剪切应力依赖性的胶原基质血小板应答增强。
综上所述,本研究为理解血小板的SHP2功能提供了新的见解,指出了与血小板信号缺陷相关的新的血栓疾病,并为有出血危险的NS患者的医疗护理提供了重要信息。
原始出处:
Marie Bellio, et al.Catalytic dysregulation of SHP2 leading to Noonan syndromes impacts on platelet signaling and functions.Blood 2019 :blood.2019001543; doi: https://doi.org/10.1182/blood.2019001543
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#功能异常#
98
#努南综合征#
70
#SHP2#
75
#综合征#
57