Eur Heart J:1型和2型心肌梗死危险因素比较!
2021-08-26 MedSci原创 MedSci原创
与1型心肌梗死相关的冠心病危险因素也是2型事件的重要预测因子。治疗这些危险因素可能会降低1型和2型心肌梗死的风险。
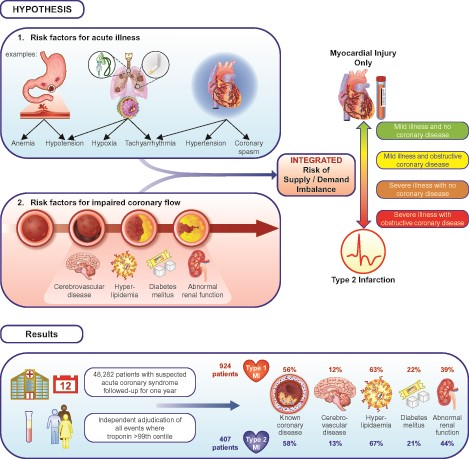
虽然动脉粥样硬化斑块破裂和血栓形成导致1型心肌梗死的危险因素已经明确,但研究人员对急性疾病期间易患2型心肌梗死的危险因素仍未明确。
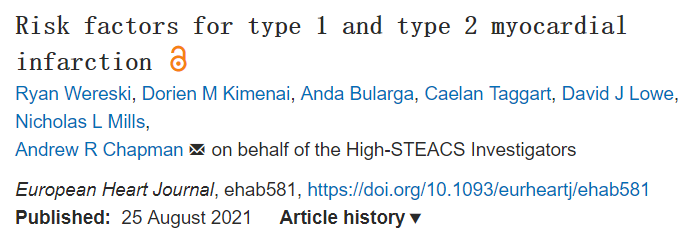
 近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在评估和比较1型和2型心肌梗死的危险因素。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在评估和比较1型和2型心肌梗死的危险因素。
 研究人员对48282名疑似急性冠状动脉综合征的住院患者组成的多中心随机试验人群进行了二次分析。首次就诊和所有随后再次就诊期间确定心肌梗死均根据心肌梗死通用定义进行判定。在1年的随访期间,Cox回归用于确定1型和2型心肌梗死的预测因子。
研究人员对48282名疑似急性冠状动脉综合征的住院患者组成的多中心随机试验人群进行了二次分析。首次就诊和所有随后再次就诊期间确定心肌梗死均根据心肌梗死通用定义进行判定。在1年的随访期间,Cox回归用于确定1型和2型心肌梗死的预测因子。
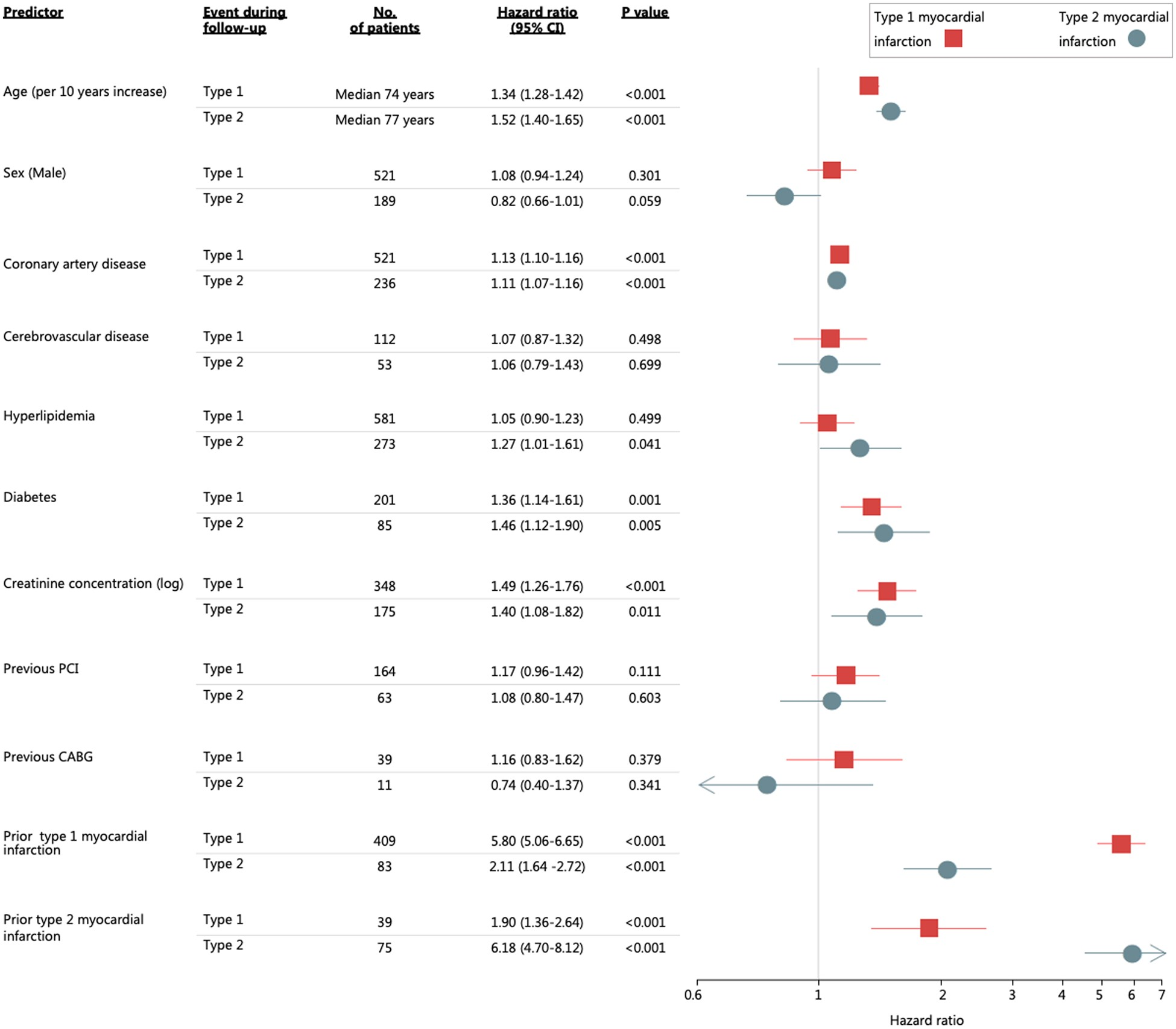 1年内,1331名患者发生了心肌梗死,其中924名和407名分别被判定为1型和2型心肌梗死。1型和2型心肌梗死的危险因素相似,包括年龄、高脂血症、糖尿病、肾功能异常和两者已知的冠心病预测因子(所有P<0.05)。虽然与1型心肌梗死相比,女性在2型心肌梗死患者中的比例更大,但在调整其他危险因素后,性别不是2型心肌梗死的预测因素[调整后的风险比(aHR)为0.82,95%置信区间(CI)为0.66-1.01]。2型心肌梗死最强预测因子是既往有2型事件的病史(aHR为6.18,95%CI为4.70-8.12)。
1年内,1331名患者发生了心肌梗死,其中924名和407名分别被判定为1型和2型心肌梗死。1型和2型心肌梗死的危险因素相似,包括年龄、高脂血症、糖尿病、肾功能异常和两者已知的冠心病预测因子(所有P<0.05)。虽然与1型心肌梗死相比,女性在2型心肌梗死患者中的比例更大,但在调整其他危险因素后,性别不是2型心肌梗死的预测因素[调整后的风险比(aHR)为0.82,95%置信区间(CI)为0.66-1.01]。2型心肌梗死最强预测因子是既往有2型事件的病史(aHR为6.18,95%CI为4.70-8.12)。
由此可见,与1型心肌梗死相关的冠心病危险因素也是2型事件的重要预测因子。治疗这些危险因素可能会降低1型和2型心肌梗死的风险。
原始出处:
Ryan Wereski.et al.Risk factors for type 1 and type 2 myocardial infarction.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab581
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











谢谢分享
68
#ART#
51
#HEART#
53
#危险因素#多谢分享。
153
收获很多
103
好文章,谢谢分享。
102