Radiology:高分辨率CT在人工耳蜗植入术中的应用
2022-01-19 shaosai MedSci原创
人工耳蜗是一种神经假体设备,是解决严重听力损失患者的有效工具。今天,即使是有功能性残余听力的患者也可以进行人工耳蜗植入。
 人工耳蜗是一种神经假体设备,是解决严重听力损失患者的有效工具。今天,即使是有功能性残余听力的患者也可以进行人工耳蜗植入。通过使用软手术技术(例如,低钻速和慢插入),可以减少手术操作所造成的创伤程度。然而,在目前的实践中,由引入异物引起的耳蜗内的长期变化既没有得到治疗,也没有得到预防。
人工耳蜗是一种神经假体设备,是解决严重听力损失患者的有效工具。今天,即使是有功能性残余听力的患者也可以进行人工耳蜗植入。通过使用软手术技术(例如,低钻速和慢插入),可以减少手术操作所造成的创伤程度。然而,在目前的实践中,由引入异物引起的耳蜗内的长期变化既没有得到治疗,也没有得到预防。
尽管人工耳蜗电极阵列通常由生物相容性聚合物制成,但它们可以通过两种途径引起炎症反应。首先,插入时的创伤可诱发急性耳蜗内组织反应,导致阵列周围形成先天性瘢痕组织。第二,自然宿主组织反应引起的延迟性炎症反应可导致阵列被包裹在纤维鞘中。随着病程的进一步发展,纤维化可以发展为新骨化。这种新骨形成(NBF)已经在动物和组织病理学研究中被观察到。然而,尚未有研究对人体内的NBF进行显示及描述。
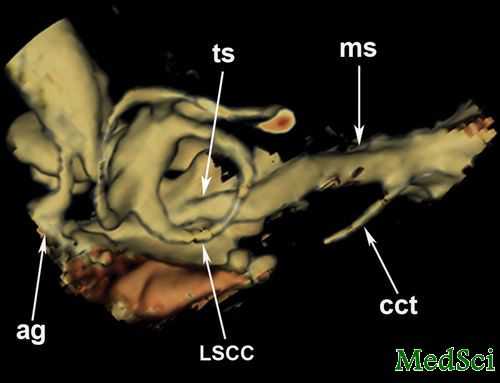
最近,随着超高空间分辨率(UHSR)CT问世,使得颞骨解剖结构更为精细的显示成为可能。近日,发表在Radiology杂志的一项研究对人工耳蜗植入患者队列中NBF的数量和位置进行了描述及统计,并测试了使用UHSR CT检测NBF的可靠性,为进一步提高人工耳蜗植入的成功率提供了影像学技术支持。
本研究于2016年12月至2018年1月期间对具有至少1年人工耳蜗植入经验的患者进行了颞骨UHSR CT扫描和残余听力评估。两位观察者独立评估了NBF的存在和位置,并使用四分法相关来评估观察者间的可靠性。此外,还评估了每个电极的标度位置。在达成共识后,参与者被分为两组:有NBF者(n = 83)和无NBF者(n = 40)。使用χ2和学生t检验来测试NBF和临床参数之间的关系,包括电极设计、手术方法和长期残余听力损失。
总共有123名参与者(平均年龄±标准差,63岁±13;63名女性)被纳入。在123名参与者中,有83人(68%)在2706个电极接触中的466个(17%)中发现了NBF。大多数NBF(466个中的428个,92%)是在10个最基底的触点周围发现的,观察者之间的一致性为86%(2683个触点中的2297个)。电极类型和手术方法之间的关联是显著的(79名参与者中的58名有NBF和预弯电极,43名中的24名有NBF和直电极,P=0.04;88名参与者中的64名有NBF和耳蜗切口方法,34名中的18名有NBF和圆窗方法,P=0.03)。全耳道插入时最不容易出现NBF,但标尺位置和NBF之间没有明显相关性(P = .15)。与没有NBF的组别相比,有NBF的组别长期残余听力损失明显较大(平均22.9 dB ± 14 vs 8.6 dB ± 18;P = .04)。
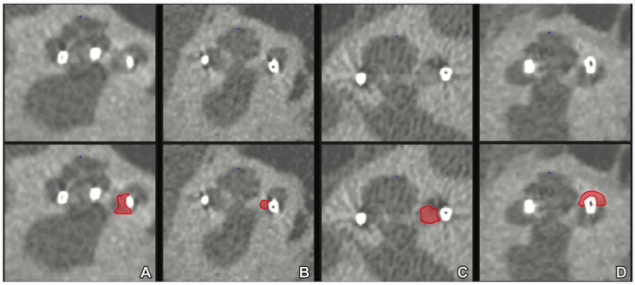
图 超高空间分辨率CT扫描图像示例图,用红色表示新骨形成(NBF)。注意NBF的不同外观,从(A)略微增加的衰减,到(D)显著的骨化。
本研究结果表明,使用超高空间分辨率CT进行人体内新骨形成(NBF)的检测是可行的,而且大多数人工耳蜗植入者在植入人工耳蜗后可能会出现NBF。这种新骨化主要位于耳蜗底部,这与更多创伤的手术参数有关。长期残余听力损失在耳蜗内骨化的患者中更为明显。
原文出处:
Floris Heutink,Tim M Klabbers,Wendy J Huinck,et al.Ultra-High-Resolution CT to Detect Intracochlear New Bone Formation after Cochlear Implantation.DOI:10.1148/radiol.211400
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#高分辨率#
153
#高分辨#
155
#人工耳蜗#
122
#植入#
112
#耳蜗植入#
98