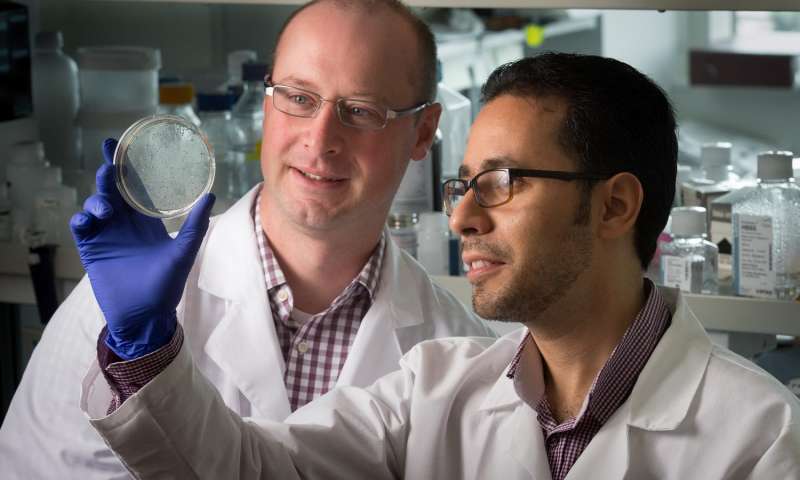
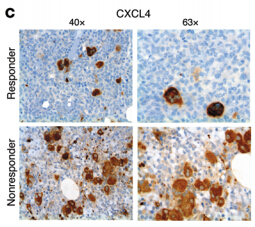
Blood:地西他滨可增强CD34+祖细胞分化的NK细胞抗白血病的活性。
2017-11-15 MedSci MedSci原创
NK细胞移植与低甲基化药物(HMA)联合,是治疗急性髓系白血病(AML)的一种具有吸引力的治疗方式。然而,目前关于HMA对NK细胞功能的影响的数据基本是来源于高于临床药物剂量的体外实验。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CD34+#
71
学习了谢谢分享!!
78
#祖细胞#
64
#细胞分化#
74
学习了
105