Cancer Discov:英国女科学家Nature之后再发白血病治疗重磅研究
2016-09-17 佚名 生物谷
最近来自英国格拉斯哥大学的科学家们在慢性髓系白血病治疗方面又取得重大进展,他们找到新的药物组合可以杀死超过90%的慢性髓系白血病干细胞。相关研究结果发表在国际学术期刊Cancer Discovery上。正常的造血干细胞发生癌变会导致慢性髓系白血病的发生,白血病干细胞会产生大量白血病细胞,如果不能得到治疗就会产生致命后果。现在慢性髓系白血病的治疗主要使用酪氨酸激酶抑制剂,但是仅接受这种治疗无法达到治

最近来自英国格拉斯哥大学的科学家们在慢性髓系白血病治疗方面又取得重大进展,他们找到新的药物组合可以杀死超过90%的慢性髓系白血病干细胞。相关研究结果发表在国际学术期刊Cancer Discovery上。
正常的造血干细胞发生癌变会导致慢性髓系白血病的发生,白血病干细胞会产生大量白血病细胞,如果不能得到治疗就会产生致命后果。现在慢性髓系白血病的治疗主要使用酪氨酸激酶抑制剂,但是仅接受这种治疗无法达到治愈疾病的效果,只能将疾病的发展控制在比较低的水平。因此许多病人需要终生维持酪氨酸激酶抑制剂治疗,但是这类药物非常昂贵,同时可能引起严重的副作用。
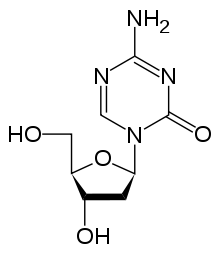
格拉斯哥大学的研究人员一直在寻找杀死慢性髓系白血病干细胞的方法,最近他们发现了一种新药物有望通过杀死慢性髓系白血病干细胞彻底治愈慢性髓系白血病,研究人员表示这种药物通过抑制EZH2的活性发挥作用。之前有研究证明EZH2能够促进多种癌细胞的存活,但是在慢性髓系白血病中没有得到研究。
文章第一作者Mary Scott表示:“我们的目标是将这种药物推向临床试验,对慢性髓系白血病病人进行治疗。目前使用EZH2抑制剂治疗其他血液癌症的临床试验已经得到一些初步结果。这种药片形式的药物非常安全同时副作用很小,非常适于慢性髓系白血病的临床治疗。”
文章作者Tessa Holyoake教授曾在今年6月份的Nature杂志上发表一项研究成果,报道了一个完全不同的药物组合可以高度有效地靶向慢性髓系白血病干细胞。
Holyoake教授说:“这篇文章以及之前Nature文章的成果表明我们一直在坚持不懈地开发新方法,寻找杀死慢性髓系白血病干细胞的新药物。”
领域内专家表示,这项研究会促进药物开发,通过靶向癌症干细胞彻底治愈这种恶性疾病。众所周知癌症复发之后再进行治疗会变得更加困难,病人的生存几率更低,这项研究找到了一种新方法可以靶向杀死那些在治疗后仍然存在并可能导致疾病复发的细胞,希望可以尽快开展临床试验验证这种治疗方法的有效性和安全性。
原始出处
Scott MT1, Korfi K1, Saffrey P2, Hopcroft LE3, Kinstrie R2, Pellicano F3, Guenther C1, Gallipoli P3, Cruz M2, Dunn K3, Jorgensen HG3, Cassels JE3, Hamilton A3, Crossan A2, Sinclair A3, Holyoake TL4, Vetrie D5.Epigenetic Reprogramming Sensitizes CML Stem Cells to Combined EZH2 and Tyrosine Kinase Inhibition.Cancer Discov.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
85
#Dis#
69
学习了,很有借鉴意义的治疗思路
109
学习了,很受益,谢谢分享,继续关注中!
103
#重磅#
80
#女科学家#
97
#ISC#
76