喜讯!罗氏乳腺癌新药Perjeta获英国NICE批准用于HER2阳性乳腺癌新辅助治疗
2017-01-05 佚名 生物谷
瑞士制药巨头罗氏(Roche)乳腺癌药物Perjeta(pertuzumab)近日在英国监管方面传来喜讯。英国国家卫生与临床优化研究所(NICE)已发布最终指南,支持将Perjeta用于英国国家服务系统(NHS),用于人表皮生长因子受体2(HER2)阳性乳腺癌患者的治疗。此次批准,使Perjeta成为英国NICE在近10年中批准的首个新的乳腺癌药物。 具体而言,NICE支持将Perjeta联

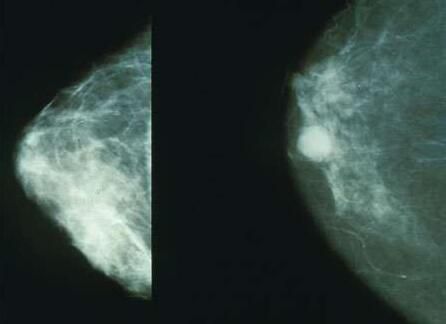
瑞士制药巨头罗氏(Roche)乳腺癌药物Perjeta(pertuzumab)近日在英国监管方面传来喜讯。英国国家卫生与临床优化研究所(NICE)已发布最终指南,支持将Perjeta用于英国国家服务系统(NHS),用于人表皮生长因子受体2(HER2)阳性乳腺癌患者的治疗。此次批准,使Perjeta成为英国NICE在近10年中批准的首个新的乳腺癌药物。
具体而言,NICE支持将Perjeta联合赫赛汀(Herceptin,通用名:trastuzumab,曲妥珠单抗)及化疗,作为一种治疗选择,用于HER2阳性局部晚期、炎症性或具有复发高风险的早期乳腺癌患者的新辅助治疗(neoadjuvant therapy,即术前治疗)。
值得一提的是,NICE在去年5月曾拒绝批准将Perjeta纳入NHS,该机构认为Perjeta的长期临床受益并不明显,并且价格昂贵不具有成本效益。此次NICE转变态度,认为在准备接受手术的乳腺癌患者中,与Herceptin+化疗相比,Perjeta联合Herceptin+化疗能够更有效地缩小乳腺和淋巴结中的肿瘤;另外,罗氏主动降价也是一个重要因素。
据估计,在英格兰和威尔士,大约有1400例HER2阳性乳腺癌患者适合Perjeta联合赫赛汀及化疗的新辅助治疗。而在苏格兰地区,苏格兰医药协会(SMC)在去年12月中旬表示,不认可Perjeta用于新辅助治疗的长期生存受益,因此该地区患者将无法通过NHS获取治疗。
Perjeta新辅助治疗:将为HER2阳性乳腺癌群体提供一种重要的治疗选择
与HER2阴性乳腺癌相比,HER2阳性乳腺癌是一种更具侵略性的乳腺癌类型,在肿瘤扩散前对HER2阳性早期乳腺癌患者进行治疗,可以提高预防疾病复发的机会。而一直以来,肿瘤的有效治疗手段都是以手术切除为主,除外科手术之外的治疗均称为辅助治疗。新辅助治疗(neoadjuvant therapy)是指在手术治疗前实施的治疗措施,主要包括化疗和放疗,其目的是减小肿瘤的体积,使其能够更容易手术移除。
在欧盟,Perjeta于2015年7月获批联合赫赛汀及化疗用于HER2阳性乳腺癌患者的新辅助治疗。来自II期临床研究NeoSphere的数据显示,术前接受Perjeta+赫赛汀+多西紫杉醇化疗方案的患者组有近40%的患者实现病理完全缓解(pCR),而术前接受赫赛汀+多西紫杉醇化疗组实现pCR的患者比例仅为21.5%;长期随访数据显示,与术前接受赫赛汀+化疗方案组相比,术前接受Perjeta+赫赛汀+化疗方案组经历疾病恶化、复发或死亡的风险降低31%(无进展生存期PFS HR=0.69; 95% CI, 0.34-1.40),经历复发或死亡的风险降低40%(无病生存期DFS HR=0.60; 95% CI, 0.28-1.27)。来自另一项II期临床研究TRYPHAENA的数据显示,接受Perjeta新辅助治疗的3个组pCR数据为54.7-63.6%。
病理完全缓解(pCR)是指在开展外科手术时受影响的乳房或乳房及局部淋巴结中检测不到肿瘤组织,即无癌状态(cancer-free)。这是评估乳腺癌新辅助治疗效果的一种常规手段,在早期乳腺癌(eBC)临床治疗中相比传统终点评估的更快。Perjeta联合赫赛汀及化疗作为一种新辅助方案在临床研究中所表现出的显著pCR疗效及长期预后受益,将为HER2阳性乳腺癌群体提供一种重要的治疗选择,将改善患者的长期预后。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
65
#新辅助#
76
#NICE#
71
#HER2阳性#
53
#英国NICE#
62