CELL:颠覆传统观念,染色质拓扑变化可抑制结直肠癌的恶性进展
2021-12-16 MedSci原创 MedSci原创
一个多世纪以来,病理学家已经观察到癌细胞核的形状、大小和染色质质地的变化。核特征有助于确定癌症的亚型和等级,对预后和治疗有重要的影响。然而,尽管它们具有诊断和临床的重要性,但我们对于这些与癌症相关的形
一个多世纪以来,病理学家已经观察到癌细胞核的形状、大小和染色质质地的变化。核特征有助于确定癌症的亚型和等级,对预后和治疗有重要的影响。然而,尽管它们具有诊断和临床的重要性,但我们对于这些与癌症相关的形态学变化的分子基础仍然知之甚少。
分子和遗传学研究已经记录了人类肿瘤中广泛的表观遗传学缺陷,包括染色质调节剂突变、DNA甲基化变化和增强子景观的改变。一些癌症中还蕴藏着调控高阶染色体结构("基因组拓扑")的蛋白质的突变,包括CTCF和cohesin亚单位。局部拓扑学改变在特定背景下驱动致癌转录程序。尽管如此,至今为止,人类肿瘤中的基因组拓扑和核组织在很大程度上是未知的。
最近,研究人员在CELL杂志发文,将结肠肿瘤和正常结肠的拓扑图与表观遗传学、转录和成像数据整合在一起,以表征染色质环、拓扑相关域和大规模隔室的改变。
为了了解核结构在癌症中是如何改变的,研究人员剖析了原发性结肠肿瘤、正常结肠和结肠癌细胞系中的基因组拓扑以及DNA甲基化、染色质修饰和CTCF。该研究的临床队列包括26个肿瘤和7个正常结肠组织样本;体外模型包括结肠癌细胞系(HCT116,SW480,RKO和LS-174T),一个来自正常结肠的系(FHC),和原代成纤维细胞(WI-38)。该研究的完整数据集包括175个库和280亿个测序读数,用于Hi-C、HiChIP、双硫酸盐测序、染色质免疫共沉淀测序(ChIP-seq)和RNA测序(RNA-seq)。
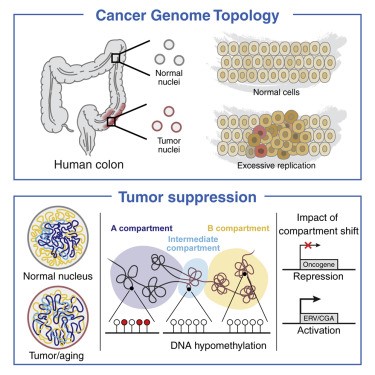
研究人员发现,在肿瘤中,开放和封闭的基因组隔室的空间分区受到了深刻的损害。这种重组伴随着隔室特异性的低甲基化和染色质变化。此外,研究人员还在肿瘤中发现了一个位于常规的A和B区室之间的界面上的区室被重组。
值得注意的是,在多次分裂的非恶性细胞中也有类似的转变。研究人员的分析还表明,这些拓扑变化在诱导抗肿瘤免疫基因的同时,也抑制了干细胞和入侵程序,因此可能抑制了恶性肿瘤的进展。
总之,以往人们认为肿瘤相关的表观基因组改变主要是致癌的,本研究对此传统观念提出了质疑。
原始出处:
Sarah E. Johnstone et al. Large-Scale Topological Changes Restrain Malignant Progression in Colorectal Cancer. CELL (2020). DOI:https://doi.org/10.1016/j.cell.2020.07.030
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
77
#Cell#
71
#结直肠#
71
#染色质#
145