JACC:心力衰竭住院患者的肾脏功能和疗效
2021-07-24 MedSci原创 MedSci原创
心力衰竭(HF)是临床常见疾病,由于其预后差,经常合并多种并发症,死亡率高,因此也是医疗中的重要疾病。
心力衰竭(HF)是临床常见疾病,由于其预后差,经常合并多种并发症,死亡率高,因此也是医疗中的重要疾病。HF 常常合并肾脏疾病,心肾相互影响,进入恶性循环,最终加快心肾功能恶化,那么其内在机制是什么呢?
来自瑞士伯尔尼大学医院的 Joerg C. Schefold 医生曾在Nature Reviews Nephrology 上,向我们展示了心衰与肾衰如何相互作用。认为心脏及肾脏疾病之间有多重共同相互作用通路,包括炎症、细胞免疫介导的免疫反应、神经内分泌机制、矿物质及骨质代谢异常等代谢营养变化、液体及酸碱平衡改变等。
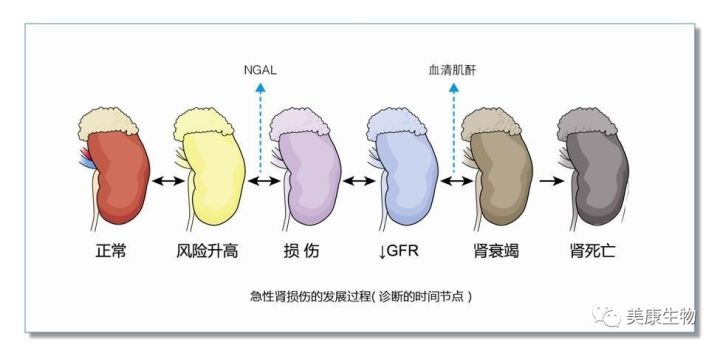
血流动力学机制包括水钠潴留引起液体超负荷,导致心肾静脉淤血。肾静脉淤血是加速肾功能不全的主要原因。神经内分泌机制包括肾素 - 血管紧张素 - 醛固酮系统(RAAS)和交感神经系统等经典代偿通路。
心衰导致肾衰的传统假说是心衰导致肾脏血流的低灌注状态。肾脏低灌注进一步引起肾血管的收缩,导致肾小管缺氧和小管坏死。此外,心输出量减少导致肾静脉高压、肾静脉淤血,加速肾脏纤维化,从而导致肾脏失功。
最近美国伊利诺伊州西北大学费恩伯格医学院医学部心脏病科的专家试图通过肾功能不全的程度来描述因HF住院的病人在护理质量和结果方面的差异。结果发表在《美国心脏病学会杂志》JACC上。
2014年至2019年,在GWTG-HF登记处的418个地点,通过出院的CKD-EPI得出的估计肾小球滤过率(eGFR),对指南指导的医疗疗法进行了评估。研究人员还评估了入院eGFR与院内死亡率的风险调整后的关系。
在365494名住院患者中(年龄72±15岁,左心室射血分数[EF]:43±17%),出院eGFR中位数为51ml/min/1.73m2(四分位数范围:34至72 ml/min/1.73m2),234332人(64%)的eGFR<60 ml/min/1.73m2,18869人(5%)接受透析治疗,eGFR分布从2014到2019保持平稳。
在157439名EF降低(≤40%)的HF患者中,出院指南指导的医疗疗法,包括β-受体阻滞剂,在出院eGFR<30 ml/min/1.73m2或透析中最低。在eGFR≥90、60-89、45-59、30-44、<30 ml/min/1.73 m2和透析的情况下,使用ACEI/ARB/ARNI+β-受体阻断剂+MRA的 "心衰三联疗法 "分别占38%、33%、25%、15%、5%和3%。
入院时eGFR较低的组别死亡率分级较高(分别为1.1%、1.5%、2.0%、3.0%、5.0%和4.2%)。在所有EF亚组中,入院eGFR和死亡率之间都有陡峭的共变因素调整的关联,但与EF中位或保留的HF相比,EF降低的HF稍强。
尽管面临着较高的死亡风险,但合并有EF值降低的HF和肾脏疾病的患者并没有得到循证医学疗法的最佳治疗,即使在eGFR水平上,这种疗法也不会因肾功能障碍而被禁忌。因此需要进一步的努力来减轻合并HF和肾脏疾病的风险。
参考文献:
Kidney Function and Outcomes in Patients Hospitalized With Heart Failure. J Am Coll Cardiol. 2021 Jul, 78 (4) 330–343
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#心力衰竭住院#
88
能学到很多知识。
73
#JACC#
60
#ACC#
62
谢谢梅斯提供这么好的信息,学到很多
95