Eur J Cancer:依维莫司联合芳香酶抑制剂是否可用作转移性乳腺癌的维持治疗?
2021-07-11 MedSci原创 MedSci原创
内分泌治疗是激素受体阳性 (HR+)/HER2- 转移性乳腺癌的主要治疗方法
虽然内分泌治疗是激素受体阳性 (HR+)/HER2- 转移性乳腺癌的主要治疗方法,但有内脏危象风险或内分泌治疗敏感性不足的患者需要接受一线化疗。在化疗停止时通常予以激素维持治疗。MAINtenance Afinitor研究是一项随机的III期试验,对比了维持依维莫司联合芳香酶抑制剂(AI)与AI单药治疗用于一线化疗后病情得以控制的转移性乳腺癌的效果。
招募了经一线化疗后病情稳定的、获得了部分缓解或完全缓解的ER+/HER2-转移性乳腺癌患者,随机分成了两组,接受依维莫司联合AI(依西美坦或来曲唑或阿那曲唑)或单纯AI治疗。主要终点是无进展生存期(PFS)。次要终点包括缓解率、安全性和总生存期。
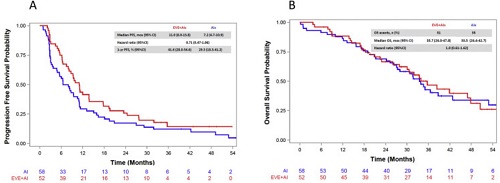
两组的PFS和OS
总体上,共有110位患者被随机分至两组:依维莫司+AI组 52位,AI组 58位。依维莫司+AI组和AI组的中位PFS分别是11.0个月和7.2个月(风险比[HR] 0.71, 95%CI 0.47-1.06)。依维莫司+AI组和AI组的客观缓解率分别是22.4%和19.2%。AI单药治疗组中报告了更高比例的疾病进展率(28.8% vs 14.3%)。联合组的中位OS是35.7个月(95%CI 26.0-47.8),单药组的中位OS是33.5个月(95%CI 26.4-42.7;HR 1.0, 95%CI 0.61-1.62)。
综上所述,依维莫司联合AI并未较单用AI显著改善一线化疗后的转移性乳腺癌患者的预后。同时考虑到治疗耐受性,内分泌维持治疗仍然是这类患者的标准疗法。
原始出处:
Guarneri Valentina,Giorgi Carlo Alberto,Cinieri Saverio et al. Everolimus plus aromatase inhibitors as maintenance therapy after first-line chemotherapy: Final results of the phase III randomised MAIN-A (MAINtenance Afinitor) trial.[J] .Eur J Cancer, 2021, 154: 21-29.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#芳香酶抑制剂#
80
#抑制剂#
71
#转移性#
78
学习
119