靶向新药伊布替尼获批新适应症——复发难治性边缘区淋巴瘤(MZL)
2017-10-17 佚名 梅斯医学
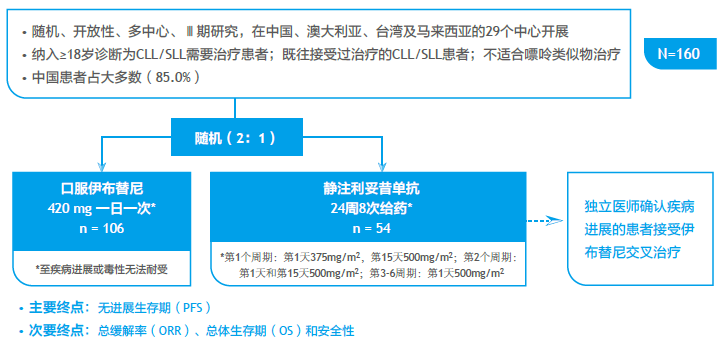
2017年1月19日,美国食品和药物管理局(FDA)已批准IMBRUVICA ?(伊布替尼)用于治疗复发难治性边缘区淋巴瘤(MZL),适用人群是那些既往使用了至少一种以抗CD20靶向药为基础方案治疗的患者。伊布替尼成为了针对“复发难治边缘区淋巴瘤”的首款FDA获批药物。MZL是一种生长缓慢的B细胞淋巴瘤,一般出现在淋巴结和各种组织的边缘(包括胃、唾液腺、甲状腺、眼睛、肺和脾脏)的白细胞中。MZL约

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#MZL#
75
#复发难治#
64
#靶向新药#
94
#伊布替尼#
72
#适应症#
80
#新适应症#
94
#边缘区淋巴瘤#
90
#难治性#
62