JCEM:妊娠期糖尿病预测子女心脏代谢标志物水平
2019-03-06 xing.T 网络
由此可见,GDM孕妇的成年后代增加了胰岛素抵抗的标志物,并且具有更容易致动脉粥样硬化的脂质谱;这些只是部分由混杂因素或当前后代的肥胖所解释。母亲孕前超重/肥胖与后代葡萄糖调节受损有关,这可通过混杂因素和/或目前的肥胖来解释。
孕产妇妊娠糖尿病(GDM)和孕前超重/肥胖(体重指数,BMI≥25kg/m2)可能对后代心脏代谢健康产生不利影响。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在评估母亲GDM和孕前超重/肥胖与成年后代心脏代谢危险因素的关系。
该研究为纵向队列研究(ESTER和AYLS),在新西兰省和芬兰北部进行,参与者平均年龄24.1岁(标准差为1.3),研究人员将后代分类,1)不论孕前BMI的GDM孕妇后代(OGDM; n=193),2)孕前超重/肥胖的正常血糖孕妇后代(ONO,n=157)和3)孕前BMI<25kg/m2的正常血糖孕妇的后代(对照组,n=556)。研究人员评估了血液中的心脏代谢生物标志物,并测量了静息血压和心率。
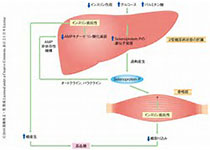
与对照组相比,OGDM和ONO具有更高的空腹血糖[1.6%(95%置信区间0.1-3.1)]和[2.3%(0.5-4.3)]以及胰岛素水平[12.7%(4.4-21.9)]和[8.7%(0.2-17.8)]。当针对混杂因素和/或当前后代特征(包括BMI或体脂百分比)进行调整时,这些差异减弱至非显著性。OGDM具有较低的性激素结合球蛋白[SHBG; 男性:-12.4%( -20.2至-3.9),女性:-33.2%( -46.3至-16.8)]、高密度脂蛋白[-6.6%( -10.9至-2.2)]和载脂蛋白A1[-4.5%(-7.5至-1.4)],这些差异在上述调整中仍然讯在。各组之间的心率和其他生物标志物相似。
由此可见,GDM孕妇的成年后代增加了胰岛素抵抗的标志物,并且具有更容易致动脉粥样硬化的脂质谱;这些只是部分由混杂因素或当前后代的肥胖所解释。母亲孕前超重/肥胖与后代葡萄糖调节受损有关,这可通过混杂因素和/或目前的肥胖来解释。
原始出处:
Nina Kaseva.et al.Gestational diabetes, but not pre-pregnancy overweight predicts cardio-metabolic markers in offspring twenty years later.J Clin Endocrinol Metab. 2019.https://doi.org/10.1210/jc.2018-02743
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#标志物#
0
#代谢标志物#
122
#JCEM#
61
#JCE#
93
#妊娠期#
79
#妊娠期糖尿病#
104
#心脏代谢#
62
谢谢MedSci提供最新的资讯
88