Cancer Cell:小分子P5091有效抵抗耐药性骨髓瘤
2012-09-14 ZinFingerNase 生物谷
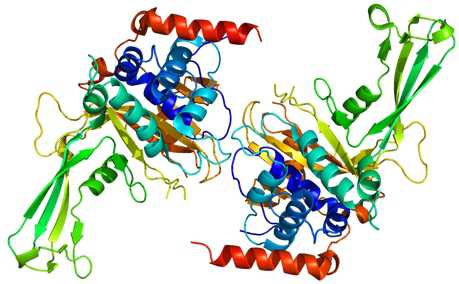
USP7蛋白结构图,图片来自维基共享资源。 来自美国达纳法伯癌症研究所(Dana-Farber Cancer Institute)的研究人员发现,一种靶向降解不需要的蛋白的细胞内复合体的分子,能够杀死对一线药物万珂(Velcade)产生耐药性的多发性骨髓瘤细胞。 根据近期刊登在Cancer Cell期刊上的一篇论文,研究人员报道,这种被称作P5091 的小分子触发在实验室培养的和动物体内的耐药

USP7蛋白结构图,图片来自维基共享资源。
来自美国达纳法伯癌症研究所(Dana-Farber Cancer Institute)的研究人员发现,一种靶向降解不需要的蛋白的细胞内复合体的分子,能够杀死对一线药物万珂(Velcade)产生耐药性的多发性骨髓瘤细胞。
根据近期刊登在Cancer Cell期刊上的一篇论文,研究人员报道,这种被称作P5091 的小分子触发在实验室培养的和动物体内的耐药性骨髓瘤细胞凋亡,即程序性细胞死亡。当研究人员把P5091与其他疗法结合使用时,这种抗骨髓瘤效应甚至更加强大。Dharminder Chauhan博士和Ze Tia博士是论文共同第一作者。
万珂是一种蛋白酶体(proteasome)抑制剂,被用来治疗多发性骨髓瘤。尽管万珂成功地治疗很多多发性骨髓瘤病人,但是随着时间的流逝,它经常丧失疗效,这就促使科学家们寻找其他的药物靶标。
蛋白酶体是细胞内的“垃圾处理工厂”,降解不想要的蛋白。抑制蛋白酶体将导致被废弃的蛋白积累,从而促进癌细胞死亡。蛋白酶体也是较大的泛素-蛋白酶体系统(ubiquitin proteasome system, UPS)的一部分。这种系统以两种方式发挥功能:它能够附着泛素到细胞蛋白上,因而将这些蛋白送到蛋白酶体进行降解;或者它移除泛素,从而让细胞不清除这些蛋白。
细胞内,很多酶有助于附着泛素到蛋白之上或移除蛋白上的泛素。在当前的研究中,研究人员着重研究一种泛素移除蛋白,即USP7。他们证实USP7作用于很多与癌症相关的蛋白:通过降解抑制癌细胞生长的蛋白,它允许肿瘤不受限制的生长。骨髓瘤细胞含有高水平USP7的病人往往具有较差的存活率。
在这项研究中,研究人员测试了一种小分子的USP7抑制剂,即P5091,是否能够导致对万珂和其他当前疗法产生抵抗性的骨髓瘤细胞凋亡。
Chauhan博士陈述道,“阻断USP7能够降低一种被称作HDM2的癌症促进蛋白的水平,其中HDM2促进抑制肿瘤细胞生长的基因p53和p21的表达。结果就是肿瘤细胞停止生长并且开始死亡。”
论文通信作者Kenneth Anderson博士说,“在实验室细胞培养物中,P5091导致骨髓瘤细胞死亡。在骨髓瘤模式动物中,这种分子破坏肿瘤生长,延长动物存活,而且不伤害正常组织。”当研究人员把P5091和药物来那度胺(lenalidomide)、辛二酰苯胺异羟肟酸(SAHA)或地塞米松(dexamethasone)结合在一起使用时,杀死骨髓瘤的效应得到显著性的改善。尽管P5091本身并没有作为药物来使用,但是这项研究证实不用靶向蛋白酶体本身,但若能够靶向泛素-蛋白酶体系统中的其他分子仍能获得杀死癌细胞的效应,同时不会产生毒性。
基于这些研究结果,Progenra公司计划在未来的临床试验中开展USP7 抑制剂的研究。

doi: 10.1016/j.ccr.2012.08.007
PMC:
PMID:
A Small Molecule Inhibitor of Ubiquitin-Specific Protease-7 Induces Apoptosis in Multiple Myeloma Cells and Overcomes Bortezomib Resistance
Dharminder Chauhan, Ze Tian, Benjamin Nicholson, K.G. Suresh Kumar, Bin Zhou, Ruben Carrasco, Jeffrey L. McDermott, Craig A. Leach, Mariaterresa Fulcinniti, Matthew P. Kodrasov, Joseph Weinstock, William D. Kingsbury, Teru Hideshima, Parantu K. Shah, Stephane Minvielle, Mikael Altun, Benedikt M. Kessler, Robert Orlowski, Paul Richardson, Nikhil Munshi, Kenneth C. Anderson
Bortezomib therapy has proven successful for the treatment of relapsed/refractory, relapsed, and newly diagnosed multiple myeloma (MM); however, dose-limiting toxicities and the development of resistance limit its long-term utility. Here, we show that P5091 is an inhibitor of deubiquitylating enzyme USP7, which induces apoptosis in MM cells resistant to conventional and bortezomib therapies. Biochemical and genetic studies show that blockade of HDM2 and p21 abrogates P5091-induced cytotoxicity. In animal tumor model studies, P5091 is well tolerated, inhibits tumor growth, and prolongs survival. Combining P5091 with lenalidomide, HDAC inhibitor SAHA, or dexamethasone triggers synergistic anti-MM activity. Our preclinical study therefore supports clinical evaluation of USP7 inhibitor, alone or in combination, as a potential MM therapy.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Cell#
62
#CEL#
56
#小分子#
46
#cancer cell#
61