J Clin Oncol:三种131I-间碘苯甲基胍方案治疗神经母细胞瘤的缓解率!
2021-07-20 MedSci原创 MedSci原创
伏立诺他和MIBG可能是真实缓解率最高的组,毒性可控
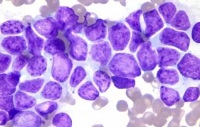
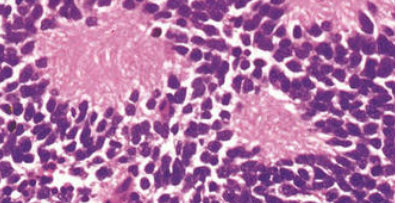
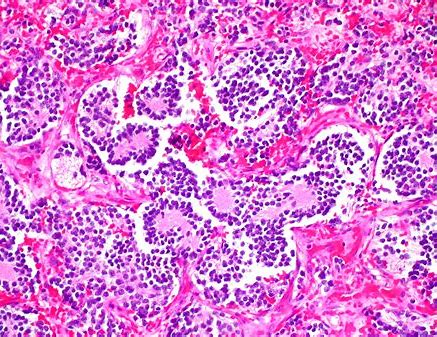
神经母细胞瘤是一种儿童癌症,通常会表达去甲肾上腺素转运体(NET)。131I-间碘苯甲基胍(MIBG)是一种有活性的神经母细胞瘤放射疗法,经NET被瘤细胞选择性的摄入。本研究旨在明确三种MIBG方案中哪一种可能与最高的真实缓解率相关。
Steven G. DuBois, et al. Randomized Phase II Trial of MIBG Versus MIBG, Vincristine, and Irinotecan Versus MIBG and Vorinostat for Patients With Relapsed or Refractory Neuroblastoma: A Report From NANT Consortium. Journal of Clinical Oncology. July 16, 2021
招募了1-30岁的复发或难治性神经母细胞瘤患者,要求至少有一个MIBG敏感部位,并有足够的自体干细胞。患者第1天接受MIBG 18 mCi/kg治疗,第15天接受自体干细胞治疗。被随机分配到A组的患者仅接受MIBG;分配到B组的患者除了接受MIBG外,在第0天接受静滴长春新碱,在第0-4天每天接受伊立替康;分配到C组的患者除了接受MIBG外,在第1天至第12天每天口服一次伏立诺他(180 mg/m2/剂)。主要终点是一疗程后的缓解率。
共招募了114位患者,其中3位不符合要求、6位无法评估,剩下105位符合要求且可评估的患者(A组 36位、B组35位、C组34位;55位男生;中位年龄6.5岁)。
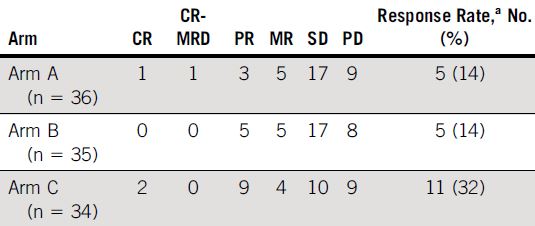
各组缓解率
一个疗程后,A组、B组和C组的缓解率(部分缓解或更好的缓解)分别是14%、14%和32%。此外,A组、B组和C组分别有5位、5位和4位患者符合神经母细胞瘤治疗新方法轻微缓解标准。最后,三组第一个疗程后任何3+级非血液学毒性的发生率分别为19%、49%和35%。
综上所述,伏立诺他和MIBG可能是真实缓解率最高的组,毒性可控。长春新碱和伊立替康似乎不能提高患者采用MIBG治疗的缓解率,并且与毒性增加有关。
原始出处:
Steven G. DuBois, et al. Randomized Phase II Trial of MIBG Versus MIBG, Vincristine, and Irinotecan Versus MIBG and Vorinostat for Patients With Relapsed or Refractory Neuroblastoma: A Report From NANT Consortium. Journal of Clinical Oncology. July 16, 2021. https://ascopubs.org/doi/full/10.1200/JCO.21.00703
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#母细胞瘤#
87
#Oncol#
83
#细胞瘤#
88
谢谢梅斯分享这么多精彩信息
118
真文章
103