“没骨气”的耳朵——复发性多软骨炎,好发于40-55岁!
2021-07-08 “西交大二附院”公众号 “西交大二附院”公众号
复发性多软骨炎 (relapsingpolychondritis, RP)是一种发作性(复发和缓解)的软骨组织进行性炎症破坏性疾病,主要累及耳、 鼻、 喉、 气管、 眼、 关节、 心脏瓣膜等器官及血管

复发性多软骨炎 (relapsingpolychondritis, RP)是一种发作性(复发和缓解)的软骨组织进行性炎症破坏性疾病,主要累及耳 鼻 喉 气管 眼 关节 心脏瓣膜等器官及血管等结缔组织, 好发于40-55岁?
RP的病因目前尚不清楚。其发病机制可能是II型胶原蛋白的自身免疫反应介导,导致机体对软骨、葡萄膜? 玻璃体心瓣膜气管黏膜下基底膜? 关节滑膜和肾小球及肾小管基底膜等含有II型胶原蛋白丰富的组织产生免疫反应?
临床表现
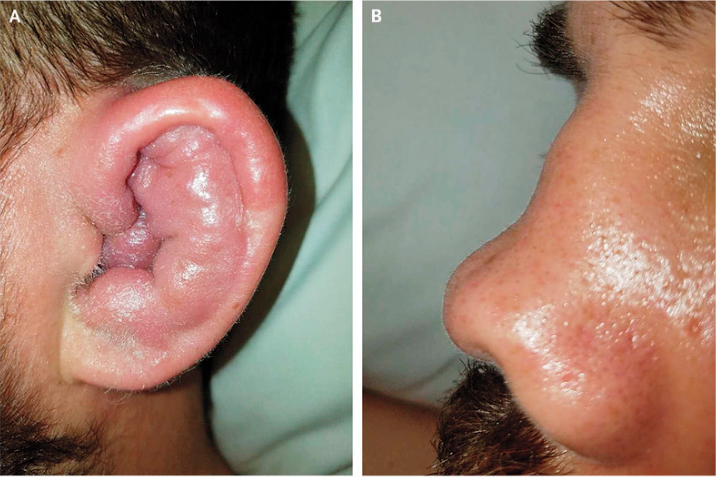
1. 耳软骨炎:耳软骨炎是最常见的临床表现,有时可侵犯外耳道,对称性受累? 初期表现为耳廓红、肿、热、痛,常在 5-10d内自行好转,后反复发作,久之耳廓塌陷畸形,表现为“花椰菜耳”;软骨变薄使血管显露表现为“蓝色耳”;外耳道狭窄、中耳炎症、咽鼓管阻塞可致传导性耳聋?
2. 鼻软骨炎:在急性期表现为局部红肿、压痛,反复发作可引起鼻软骨局限性塌陷,发展为鞍鼻畸形?
3. 眼部病变:最常见的临床表现为上眼睑下垂、眼睑水肿、结膜炎、巩膜炎、角膜炎及葡萄膜炎;严重者表现为视网膜动脉和静脉阻塞、视神经炎、视网膜病变和视网膜脱离,但较少见。
4. 关节表现:血清阴性寡/多关节炎,无破坏性及侵袭性,受累关节分布表现为不对称性;另外腱鞘炎也有少量报道。
5. 呼吸系统表现:多达一半患者会出现呼吸系统问题,大多表现为喉软骨炎(声音嘶哑、气管环压痛、咳嗽、呼吸困难和痉挛),其余肺部表现为气道前壁增厚、局部或弥漫性气道狭窄以及气管支气管软化。局部声门下狭窄较少见。呼吸道并发症及肺部感染是死亡最常见的原因。
6. 心血管系统表现:仅次于呼吸系统表现的第二大死亡原因,最常见的心血管表现是由主动脉根动脉瘤样变所致的主动脉反流,其他表现为二尖瓣反流、窦性心动过速、不同程度的房室传导阻滞、心包炎、心肌炎、血管炎和血栓形成性静脉炎。
7. 皮肤表现:紫癜、丘疹和结节,在复发性多软骨炎中很常见,局部血管炎也可导致口腔及皮肤溃疡。口腔和生殖器溃疡、其他白塞病相关表现及软骨炎,也被称为MAGIC综合征。分布在躯干及肩膀的环状、爆发性荨麻疹被认为是RPC特有的皮肤表现,但这种皮疹要警惕骨髓增生异常综合征。
8. 神经系统表现:最常见的神经系统表现是第5和第7根颅神经麻痹,其他表现为脑膜炎、脑炎和动脉瘤等。
9. 肾脏表现:受累少,一旦受累表明预后较差。最常见的表现为系膜增生性肾小球肾炎,随后发展为节段性坏死性肾小球肾炎。IgA肾病和间质性肾炎也有报道。
诊断治疗
根据典型的临床表现和实验室检查在考虑RP的可能时,可按1975年McAdam 的诊断标准:
1、双耳软骨炎;
2、非侵蚀性多关节炎;
3、鼻软骨炎;
4、眼炎,包括结膜炎、角膜炎、巩膜炎、浅层巩膜炎及葡萄膜炎等;
5、喉和(或)气管软骨炎;
6、耳蜗和(或)前庭受损,表现为听力丧失、耳呜和眩晕。
具有上述标准3条或3条以上者可以确诊。
通常的治疗药物包括NSAIDs、激素及甲氨蝶呤、环磷酰胺、硫唑嘌呤、环孢素等免疫抑制剂;近年来,发现一些生物制剂对严重病例有效,并可能阻止病情进展:TNFα抑制剂(阿达木单抗等)、IL-6抑制剂(托珠单抗)、抗CD20(利妥昔单抗)、抗IL1(阿那白制素)和t细胞共刺激/激活抑制剂(阿巴西普)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#复发性多软骨炎#
69
#软骨炎#
65
#复发性#
60
学习了
84
学习了
105
#学习#学习了
72