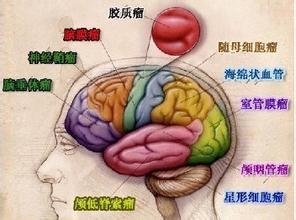
Oncotarget:中性粒细胞与淋巴细胞比值预测神经胶质瘤患者生存情况!
2017-08-13 Emma MedSci原创
神经胶质瘤,是发生于神经外胚层的肿瘤。大多缓慢发病,自出现症状至就诊时间一般为数周至数月,少数可达数年。恶性程度高的和后颅窝肿瘤病史较短,较良性的或位于静区的肿瘤病史较长。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#患者生存#
46
#target#
52
学习了,谢谢分享
89
签到学习了!……
76
#中性粒细胞#
43
#淋巴细胞#
36
#神经胶质瘤#
68
神经胶质瘤系浸润性生长物,它和正常脑组织没有明显界限,难以完全切除,对放疗化疗不甚敏感,非常容易复发,手术难以切除或根本不能手术。
73
不错的,学习了,谢谢分享!
84
优质资源
75