Circulation: PCSK9抑制剂还能抗栓!
2020-04-04 朱朱 中国循环杂志
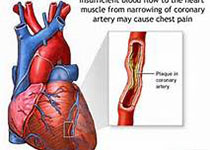
PCSK9抑制剂是一类新型降胆固醇药物。近期Circulation杂志发表的一项研究表明,PCSK9抑制剂可能还有抗栓功能。
PCSK9抑制剂是一类新型降胆固醇药物。近期Circulation杂志发表的一项研究表明,PCSK9抑制剂可能还有抗栓功能。
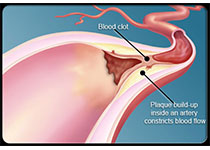
研究者发现,PCSK9抑制剂可显著降低静脉血栓栓塞风险,该作用一定程度上可能是通过降低脂蛋白(a)水平而实现的。
研究者首先对FOURIER研究进行了事后分析,发现在该研究中,应用evolocumab的第一年,静脉血栓栓塞风险并未显著降低,但1年后显著降低了46%。
研究人员还对FOURIER研究和ODYSSEYOUTCOMES研究进行了meta分析,发现应用PCSK9抑制剂的患者静脉血栓栓塞风险降低了31%。
该研究还显示,PCSK9抑制剂对静脉血栓栓塞风险的降低幅度与患者基线低密度脂蛋白胆固醇(LDL-C)水平无关,而基线脂蛋白(a)水平与之可能有关。
在基线脂蛋白(a)水平较高的患者中,evolocumab将脂蛋白(a)水平降低了33 nmol/L,静脉血栓栓塞风险降低了48%;而在基线脂蛋白(a)水平较低的患者中,evolocumab仅将脂蛋白(a)水平降低了7 nmol/L,对静脉血栓栓塞风险并无降低作用。
进一步分析显示,基线脂蛋白(a)水平与静脉血栓栓塞风险降低幅度有明显关联。
研究者利用FOURIER研究进行遗传分析后发现,多基因风险评分可确定静脉血栓栓塞风险增加超过2倍的患者,以及从evolocumab治疗中获益较大的患者。
原始出处:
Nicholas A, et al. The Effect of PCSK9 Inhibition on the Risk of Venous Thromboembolism. Circulation, Originally published 29 Mar 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PCS#
108
#PCSK9抑制#
97
#Csk#
67
学习了
114
#抑制剂#
0
学习了
108