JAMA Cardiol:左心室和主动脉收缩压峰值时间与主动脉瓣狭窄严重程度和主动脉瓣钙化的关联
2019-05-05 xiangting MedSci原创
TLV-Ao延长与严重AVC相关。这个基于导管的血液动力学指标可作为区分低梯度严重AS的另一个替代指标。
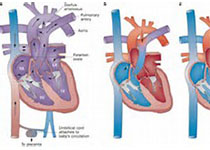
低梯度严重主动脉瓣狭窄(AS)的诊断具有挑战性。这项研究假设左心室(LV)和主动脉收缩压峰值之间的时间(TLV-Ao)与主动脉瓣狭窄(AS)的严重程度相关,并且在诊断严重AS时具有附加价值,尤其是低梯度AS患者。
这项研究旨在探讨严重AS患者中测量导管TLV-Ao的诊断价值。
研究人员在克利夫兰诊所基金会(一个三级转诊中心)研究了123名严重AS患者,这些患者通过股动脉入路接受经导管主动脉瓣置换术(TAVR),并进行了TAVR前心脏CT评估和TAVR术中血流动力学测量。所有患者均通过多检测器CT接受血流动力学评估、超声心动图评估和主动脉瓣钙化(AVC)量化。在TAVR前通过左心导管收集血液动力学数据,并且离线计算TLV-Ao。在2015年10月5日至2016年7月20日期间进行数据分析。
分析了TLV-Ao与AVC或其他常规成像参数之间的关联。
纳入患者的平均(SD)年龄为81(9)岁,65名(54%)为男性。在123名患者中,48名患者(39%)为低梯度AS(<40mmHg)和平均(SD)TLV-Ao为69(39)毫秒。在多因素logistic回归分析中,TLV-Ao大(优势比[OR],1.02;95%CI,1.01-1.04;P= .002)和主动脉瓣(AV)峰值速度快(OR,1.01; 95%CI,1.00-1.02; P= .008)与严重AVC(AVC>1000AU)独立相关。将TLV-Ao加入峰值AV速度和AV面积显示出与AVC相关的明显增量值,净重新分类改善为0.61(95%CI,0.23-0.99; P= .002)和综合辨别力改善为0.09(95%CI,0.03-0.16;P = .003)。在低度AS患者亚组中,较高的TLV-Ao是与严重AVC相关的唯一参数(OR,1.02; 95%CI,1.001-1.04;P= .03)。
原始出处:
Kimi Sato. Association of Time Between Left Ventricular and Aortic Systolic Pressure Peaks With Severity of Aortic Stenosis and Calcification of Aortic Valve. JAMA Cardiology. 01 May 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#收缩压#
87
#Cardiol#
85
#主动脉收缩压#
81
#主动脉瓣#
79
#左心室#
72
#主动脉#
80
#主动脉瓣钙化#
81