非随机实验性研究、诊断性试验及动物实验的质量评价工具
2019-02-14 曾宪涛,庄丽萍,杨宗国,董圣杰 中国循证心血管医学杂志
非随机实验性研究(non-randomized experimental study)和诊断准确性试验的Meta分析是临床研究重要组成 部分,而临床前的动物实验的Meta分析也日渐得到重视,其 结论已成为循证决策的依据之一。在前面的章节中,我们已 对随机对照试验[1] 及观察性研究[2] 的质量评价工具进行了简 介,现对较为常用的或推荐使用的非随机实验性研究、诊断 准确性试验及
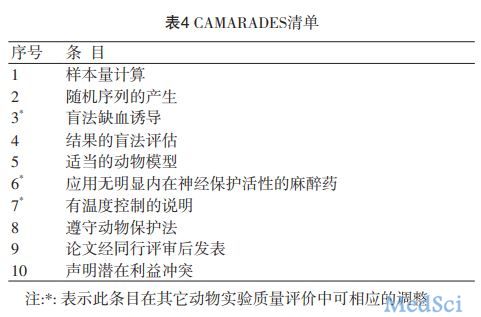
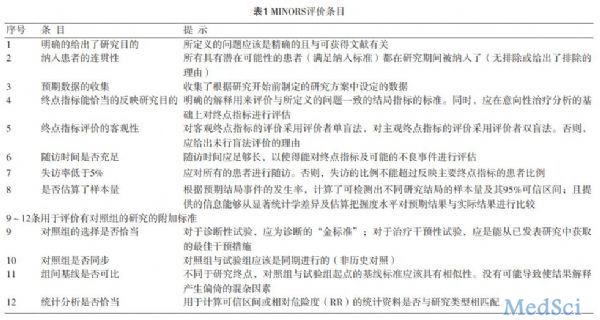
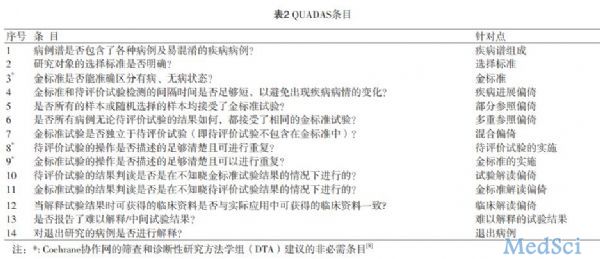
非随机实验性研究(non-randomized experimental study)和诊断准确性试验的Meta分析是临床研究重要组成 部分,而临床前的动物实验的Meta分析也日渐得到重视,其 结论已成为循证决策的依据之一。在前面的章节中,我们已 对随机对照试验[1] 及观察性研究[2] 的质量评价工具进行了简 介,现对较为常用的或推荐使用的非随机实验性研究、诊断准确性试验及动物实验的评价工具进行简介。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#实验性#
93
#诊断性试验#
83
#诊断性#
97
好
114
#评价#
98
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦
114
好!!!!!
106
优秀!
114
学习了,谢谢作者分享!
106
好好好好好好
104